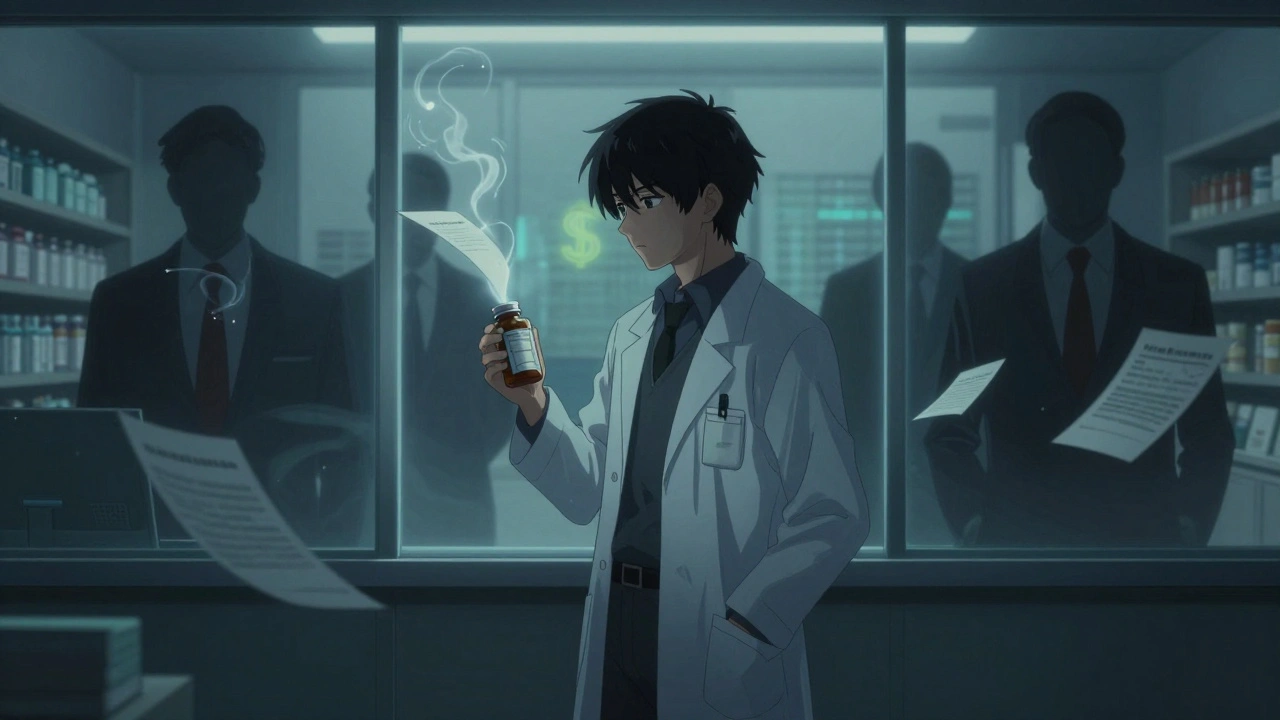
Pharmaceutical Competition: How Generic Drugs, Patents, and Pricing Shape Your Medications
When you hear pharmaceutical competition, the battle between brand-name drug makers and generic manufacturers over market share, pricing, and access. Also known as drug market rivalry, it directly impacts whether you pay $10 or $300 for the same pill. This isn’t just corporate drama—it’s why your prescription might switch from Viagra to generic sildenafil without you even noticing.
Generic drugs, bioequivalent versions of brand-name medications approved by the FDA after patents expire are the main weapon in pharmaceutical competition. They’re not cheaper because they’re lower quality—they’re cheaper because no one’s paying for ads, celebrity endorsements, or decades of R&D anymore. But here’s the catch: not all generics enter the market at once. Patent expiration, the legal end of a drug maker’s exclusive right to sell a medication triggers a race. The first generic company to file an ANDA with the FDA often gets 180 days of exclusive sales—a loophole that keeps prices high until more players jump in. That’s why you might see one generic version of a drug for months, then suddenly five more appear.
Drug pricing, what you pay at the pharmacy counter, shaped by negotiations between manufacturers, insurers, and pharmacy benefit managers is the real battleground. In the U.S., drugmakers can set prices almost anywhere because there’s no government cap. That’s why Americans pay three times more than people in Canada or the UK for the same pills. Meanwhile, FDA approval, the process that certifies a drug is safe and effective before it hits the market doesn’t just apply to new drugs—it’s the gatekeeper for generics too. Tentative approval lets companies prepare to launch right when the patent dies, but lawsuits can delay it for years. That’s why some generic versions never arrive, and patients are stuck with expensive brands.
Pharmaceutical competition doesn’t just affect your wallet. It affects your safety. When a company rushes a generic to market to beat the 180-day window, quality control can slip. That’s why counterfeit drugs and substandard generics show up in developing nations—and sometimes even in U.S. online pharmacies. On the flip side, competition drives innovation. AI now helps predict which drugs will face the fiercest generic challenges, and pharmacogenomics lets pharmacies match you with the right generic based on your genes. Meanwhile, hospitals use formularies to pick the cheapest effective option, and digital tools track whether you’re actually taking your cheaper meds.
What you’ll find below isn’t just a list of articles—it’s a map of how this system works in real life. From how patent litigation delays life-saving generics to why your doctor might switch your blood pressure med to a cheaper version, these stories show the hidden forces behind your prescription bottle. You’ll learn how to spot safe online pharmacies, why your ADHD meds might be linked to heart risks, and how flavoring kids’ pills can boost adherence by 40%. This is pharmaceutical competition not as a business term—but as something that touches your health, your money, and your daily life.
Economic Impact of Patent Expiration: When Drug Prices Drop
When pharmaceutical patents expire, drug prices typically drop by 80% or more as generics enter the market-but corporate tactics like patent thickets can delay savings for years. Learn how this affects your out-of-pocket costs.
Antitrust Laws and Competition Issues in Generic Pharmaceutical Markets
Antitrust laws in the generic drug market prevent branded companies from blocking cheaper alternatives through pay-for-delay deals, sham petitions, and product hopping. These tactics cost consumers billions and limit access to essential medicines.
© 2026. All rights reserved.