Stimulant Cardiac Risk Assessment
Assess Your Cardiac Risk
This tool helps you understand your potential cardiac risk when taking stimulant medications. Results are for informational purposes only and should not replace medical advice.
When you or your child starts taking ADHD medication like Adderall or Ritalin, the goal is simple: focus better, feel calmer, get things done. But what if that same pill could quietly mess with your heart? It’s not a scare tactic - it’s a real, documented risk. Stimulants used for ADHD can trigger irregular heartbeats, especially in certain people. And while most users never have a problem, ignoring the possibility can be dangerous. The key isn’t avoiding these medications entirely - it’s knowing who is at risk and how to manage it safely.
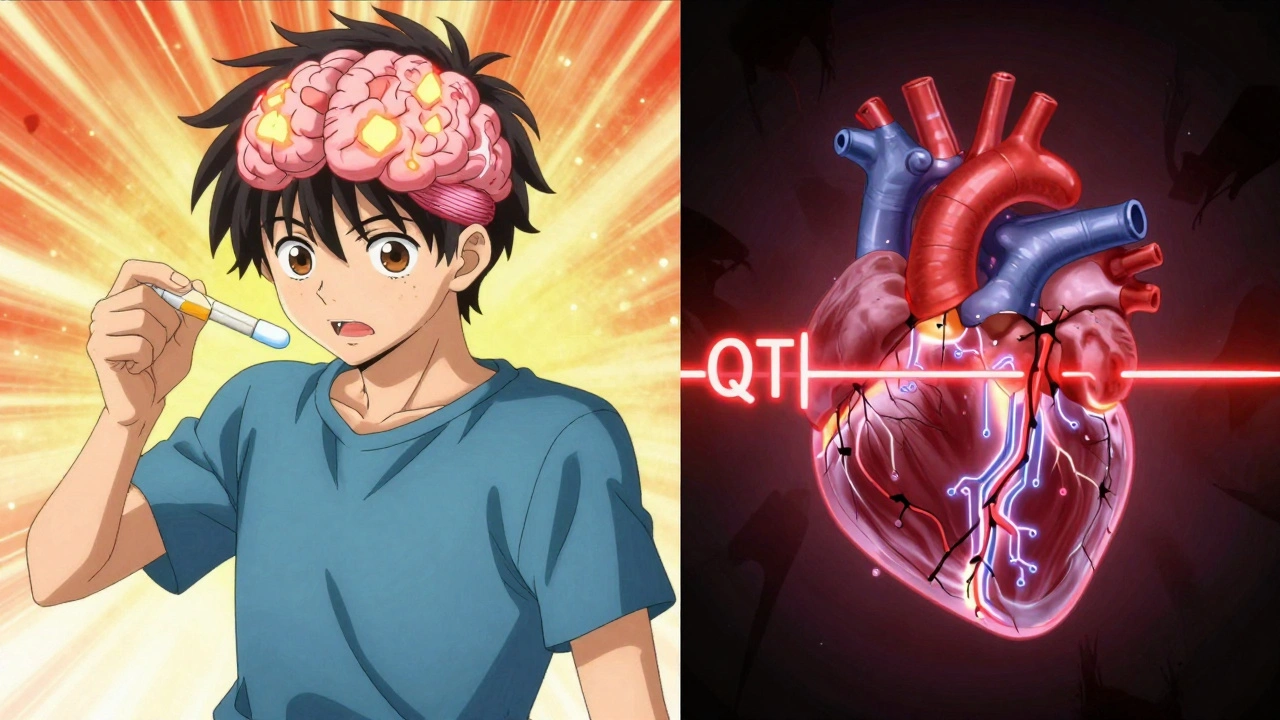
How Stimulants Affect the Heart
Prescription stimulants like amphetamines (Adderall, Vyvanse) and methylphenidate (Ritalin, Concerta) work by boosting dopamine and norepinephrine in the brain. That’s what improves focus. But those same chemicals also hit the heart. They make it beat faster and push blood harder through the arteries. For most healthy people, this is a minor, temporary change - maybe a pulse that’s 5 beats per minute higher, a slight rise in blood pressure. Nothing to panic about.
But for some, it’s more than that. These drugs can interfere with the heart’s electrical system. They block potassium and sodium channels that control how heart cells recharge between beats. When those channels get blocked, the heart’s rhythm can go off-track. This isn’t just theory - studies show stimulants can prolong the QT interval on an ECG, a sign the heart is taking longer than normal to reset. A prolonged QT interval increases the chance of dangerous arrhythmias like torsades de pointes, which can lead to sudden cardiac arrest.
The risk isn’t the same for everyone. Illicit drugs like cocaine and methamphetamine are far worse. They don’t just tweak the system - they wreck it. Cocaine blocks multiple ion channels at once, causes rapid heart rate spikes, and leads to heart muscle scarring over time. Methamphetamine does the same, but even more aggressively. People who use these drugs have 2.5 to 4.5 times higher rates of ventricular arrhythmias than non-users. Prescription stimulants? The risk is much lower - but still real, especially in older adults or those with hidden heart conditions.
Who’s at Highest Risk?
Not everyone taking ADHD meds needs to worry. But some groups should be extra cautious.
- Adults over 65: A 2021 study found that seniors starting stimulants had a threefold increase in ventricular arrhythmias within the first 30 days. The heart changes with age - less flexibility, weaker electrical signaling. Adding stimulants can push it over the edge.
- People with personal or family history of sudden cardiac death: If a close relative died unexpectedly before age 50, or if you’ve had unexplained fainting spells, that’s a red flag. Some inherited conditions like long QT syndrome or hypertrophic cardiomyopathy can be silent until a stimulant triggers a crisis.
- Those with known heart disease: Congenital defects, prior heart attacks, or diagnosed arrhythmias like atrial fibrillation mean your heart is already under stress. Stimulants add fuel to the fire.
- People on multiple medications: If you’re taking antidepressants, antipsychotics, or antibiotics that also affect heart rhythm, combining them with stimulants can create dangerous interactions.
Here’s the catch: many of these conditions show no symptoms until something triggers them. That’s why a routine physical isn’t enough. You need to dig deeper.
How Doctors Assess Your Risk
Most doctors don’t order an ECG before prescribing stimulants - and that’s by design. The American Heart Association and American Academy of Pediatrics agree: routine ECGs aren’t necessary for everyone. But they do recommend a careful history and physical.
Here’s what a good risk assessment includes:
- Personal history: Have you ever had chest pain, dizziness, fainting, or palpitations? Especially during exercise? These aren’t just ‘nerves’ - they’re warning signs.
- Family history: Did any close relative die suddenly before age 50? Or have a known heart condition like long QT syndrome or Brugada syndrome? That’s critical info.
- Physical exam: The doctor listens for heart murmurs, checks your pulse for irregularity, and measures your blood pressure. A murmur could mean an undiagnosed structural problem.
- Medication review: Are you on anything else that affects heart rhythm? Even over-the-counter cold medicines can interact.
If any red flags come up - fainting, family history of sudden death, abnormal heart sounds - the next step is an ECG. If the ECG shows QT prolongation or other abnormalities, a cardiologist should be involved before starting any stimulant.
After starting the medication, monitoring continues. Blood pressure and heart rate are checked within 1-3 months, then every 6-12 months. If your BP climbs above the 95th percentile for your age, or if you develop palpitations, the drug may need to be stopped.
The Evidence Is Mixed - So What Should You Believe?
You’ve probably heard conflicting things. One study says stimulants triple arrhythmia risk. Another says there’s no significant link. Which one’s right?
The truth is, both can be true - depending on who you are.
A 2022 meta-analysis in JAMA Network Open looked at over a million children and young adults and found no statistically significant rise in cardiovascular events overall. That’s reassuring for most families. But a 2021 study in PubMed Central focused on older adults and found a clear spike in ventricular arrhythmias in the first month after starting stimulants. And a 2025 study in the European Heart Journal showed that chronic cocaine and meth use causes permanent electrical damage to the heart.
So the picture isn’t black and white. For healthy teens and young adults with no heart issues, the risk of a serious event is extremely low - estimated at less than 1 in 100,000 per year. But for older adults, those with hidden heart conditions, or those using illicit stimulants? The risk jumps dramatically.
The bottom line: don’t dismiss the concern. Don’t panic either. Use the tools available - history, physical, targeted testing - to figure out where you stand.
Non-Stimulant Alternatives for ADHD
If your heart is a concern, you’re not out of options. Non-stimulant medications exist and can work well - just not as fast or as powerfully.
- Atomoxetine (Strattera): This is a norepinephrine reuptake inhibitor. It doesn’t cause the same heart rate spikes as stimulants. Studies show it helps about 50-60% of users - less than stimulants’ 70-80%, but still effective. Side effects include nausea, fatigue, and occasional liver enzyme changes.
- Guanfacine (Intuniv) and Clonidine (Kapvay): These are blood pressure medications repurposed for ADHD. They work by calming overactive brain circuits. They’re especially helpful for people with ADHD and anxiety or sleep issues. They don’t raise heart rate - in fact, they lower it slightly. Downsides? Drowsiness, dizziness, and sometimes low blood pressure.
These drugs take weeks to build up in your system. You won’t feel an instant change like you do with Adderall. But they’re much safer for the heart. Many patients who can’t tolerate stimulants find these a good middle ground - especially when combined with behavioral therapy.
When to Stop Stimulants
Not every elevated BP or skipped beat means you need to quit. But there are clear red flags:
- Resting heart rate consistently above 100 bpm
- Blood pressure above the 95th percentile for age and height
- Unexplained fainting or near-fainting
- Palpitations that feel like fluttering, pounding, or skipping
- ECG showing QT interval longer than 460 milliseconds
- New diagnosis of structural heart disease
If any of these happen, talk to your doctor immediately. Don’t stop the medication cold turkey - that can cause withdrawal symptoms. But don’t wait either. A quick ECG and cardiology consult can prevent a serious event.
What’s Changing in 2025?
Guidelines are evolving. The American College of Cardiology is finalizing new recommendations expected in late 2025. They’ll likely push for more personalized risk scoring - not just age or family history, but genetic markers too. Early research is looking at variations in adrenergic receptor genes that might make some people more sensitive to stimulant effects.
For now, the message is clear: stimulants are still first-line treatment for ADHD. For most people, the benefits far outweigh the risks. But that doesn’t mean we treat everyone the same. The future isn’t about banning these drugs - it’s about matching the right person with the right treatment. If your heart is healthy, stimulants can be life-changing. If your heart has hidden vulnerabilities, there are safer paths forward.
Can stimulants cause sudden cardiac death?
Yes, but it’s extremely rare in healthy individuals. Most cases involve people with undiagnosed heart conditions like long QT syndrome or hypertrophic cardiomyopathy. The absolute risk for children and teens without heart problems is less than 1 in 100,000 per year. For older adults or those with known heart issues, the risk is higher - but still low overall. Screening and monitoring reduce this risk significantly.
Do I need an ECG before starting ADHD medication?
Not routinely. Major guidelines from the American Heart Association and American Academy of Pediatrics say a detailed medical history and physical exam are enough for most people. But if you have symptoms like fainting, chest pain, or a family history of sudden cardiac death, an ECG is recommended. Many doctors now do one anyway for older patients or those on high doses.
Are non-stimulant ADHD meds as effective?
They’re generally less effective than stimulants. Stimulants help about 70-80% of users; non-stimulants like Strattera or Intuniv help 50-60%. But they’re still meaningful for many people, especially those who can’t tolerate stimulants due to heart concerns, anxiety, or sleep issues. They take longer to work - weeks, not days - but they’re safer for long-term use in high-risk patients.
Can I drink caffeine while taking stimulants?
It’s not recommended. Caffeine is also a stimulant. Combining it with ADHD meds can increase heart rate and blood pressure beyond safe levels, raising the risk of palpitations or arrhythmias. Most doctors advise limiting caffeine to one cup of coffee or less per day - and avoiding energy drinks entirely.
What should I do if I feel my heart racing after taking my ADHD pill?
Stop taking the medication and contact your doctor right away. Don’t wait to see if it gets better. Record how long the racing lasted, whether you felt dizzy or short of breath, and if it happened after a dose increase. Your doctor may order an ECG or refer you to a cardiologist. In many cases, lowering the dose or switching to a non-stimulant resolves the issue.
Next Steps: What to Do Now
If you’re currently on stimulants and have no heart symptoms or family history, keep taking them as prescribed and stick to your follow-up appointments. Monitor your pulse and blood pressure at home if you can - even simple tracking helps your doctor spot trends.
If you’ve never been screened and you’re over 40, have high blood pressure, or have a family history of sudden cardiac death, talk to your doctor about getting an ECG. It’s a quick, painless test that can give you peace of mind.
If you’re considering stimulants for the first time and have heart concerns, ask about non-stimulant options. They’re not perfect, but they’re safer for your heart - and sometimes, that’s worth the trade-off.
The goal isn’t to avoid ADHD treatment. It’s to get the right treatment - the one that helps you focus without putting your heart at risk.



9 Comments
vinoth kumar
December 2, 2025 AT 20:33Really appreciate this breakdown. I’m a dad in India whose kid started on Vyvanse last year, and I was terrified about the heart stuff until I read this. We got an ECG just to be safe - totally normal. Now we monitor pulse at home weekly. No issues, but knowing the risks made all the difference. Thanks for not just scaring people but giving real tools.
Gene Linetsky
December 4, 2025 AT 03:54They’re lying to you. Big Pharma doesn’t care if your kid’s heart gives out - they just want you hooked on $200/month pills. The FDA knows stimulants cause arrhythmias, but they won’t ban them because the drug companies fund their conferences. You think your doctor’s looking out for you? Nah. He’s on their payroll. Get off the meds. Try meditation. Or better yet - stop pretending your kid has ADHD. He’s just bored.
Ignacio Pacheco
December 5, 2025 AT 19:41So let me get this straight - you’re telling me that a drug that makes my brain work better might also make my heart explode… but only if I’m old, or have a secret genetic time bomb, or take cold medicine? And the solution is… more tests? More doctors? More paperwork? Cool. So basically, if I’m healthy, young, and don’t have a family history of sudden death before 50, I’m fine. But if I’m 45 and had a weird dizzy spell once in 2012? I’m basically a walking time bomb. Thanks for that clarity.
Jim Schultz
December 6, 2025 AT 13:58Let’s be real: the only people who need to worry about stimulant-induced arrhythmias are those who didn’t bother to get a baseline ECG, didn’t disclose their 12-year-old cousin’s sudden cardiac death, and then downed three Red Bulls before their first Adderall dose. You’re not ‘at risk’ - you’re just negligent. The science is clear. The guidelines are clear. If you’re skipping the basics, you’re not a patient - you’re a liability. And yes, I’ve read every single study cited here. Twice.
Kidar Saleh
December 6, 2025 AT 23:38In the UK, we’ve seen a quiet revolution in ADHD care over the past five years. GPs are far more cautious now. We don’t just hand out prescriptions like candy. We screen, we educate, we follow up. And we’re seeing fewer cardiac events - not because stimulants are dangerous, but because we treat them like the powerful tools they are. This isn’t fear-mongering. It’s responsibility. And it’s working.
Chloe Madison
December 7, 2025 AT 13:05As a nurse who’s worked in pediatric cardiology for 14 years - I can’t tell you how many parents come in panicked because their kid’s heart rate went from 80 to 95 after starting Ritalin. And guess what? That’s normal. It’s not dangerous. But I also can’t tell you how many kids we’ve saved because a parent asked, ‘Wait - my uncle died at 42 from a heart thing…’ - and we ran the ECG. That’s the difference between fear and awareness. You’re not overreacting if you ask. You’re being smart.
Vincent Soldja
December 8, 2025 AT 18:09Stimulants bad. Heart bad. Avoid.
Makenzie Keely
December 10, 2025 AT 17:22Thank you for writing this with such precision - and for including the 2025 ACC guidelines preview. I’ve been waiting for someone to clarify the nuance between population-level risk and individual risk. So many people either panic or dismiss this entirely. But the truth? It’s a spectrum. And the non-stimulants? They’re not ‘second-tier’ - they’re ‘right-tier’ for the right person. I’ve seen patients thrive on Strattera after years of stimulant-induced palpitations. It’s not about ‘better’ - it’s about ‘appropriate.’ And that’s what this article nails.
Francine Phillips
December 11, 2025 AT 21:20My doc prescribed Adderall without asking about my family. My dad died at 48 of something they never diagnosed. Now I’m on guanfacine. It’s slower. But I’m alive.