When you hurt - whether it’s a bad back, a sprained ankle, or chronic knee pain - the first thing most people think is: pain medication. But not all pain meds are created equal. Some work fast, but come with hidden dangers. Others take a little longer, but keep you safer over time. The big divide? Opioids and non-opioids. And the evidence now clearly shows that for most people, non-opioids are the smarter, safer first choice.
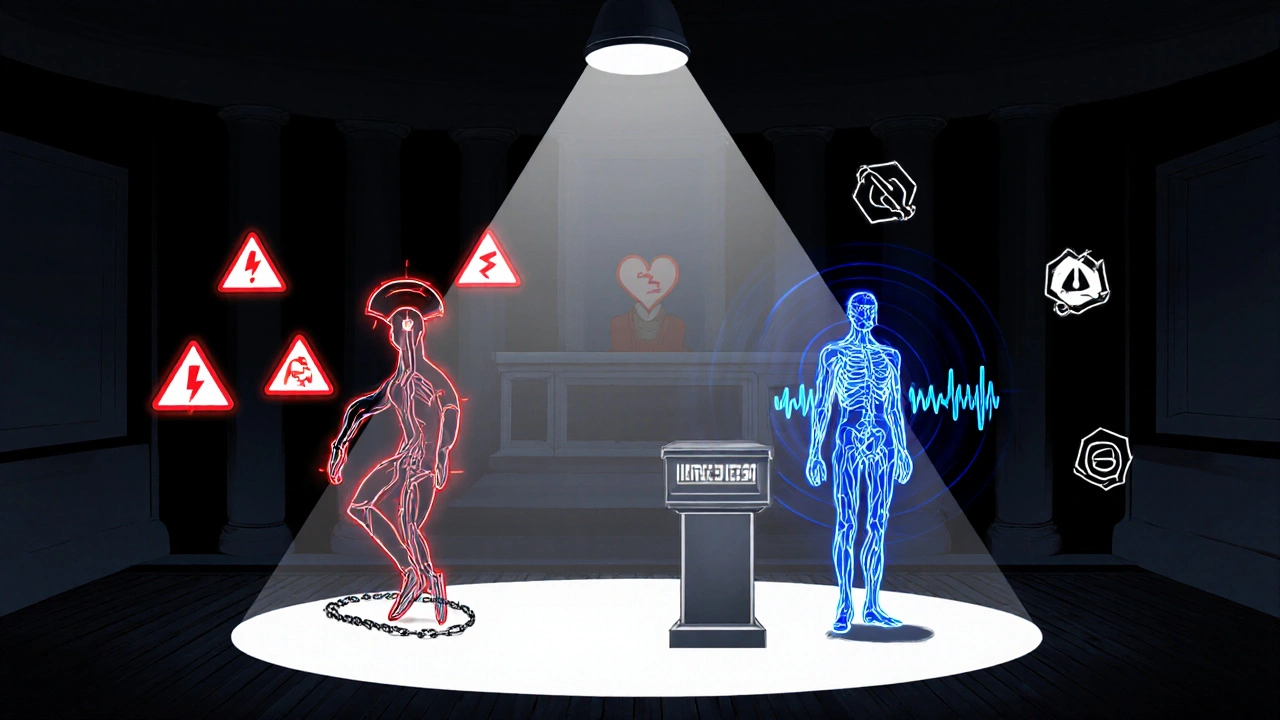
What Are Opioids, Really?
Opioids are powerful drugs that bind to special receptors in your brain and spinal cord to block pain signals. They include prescription pills like oxycodone, hydrocodone, and morphine, as well as illegal drugs like heroin. They were once seen as the gold standard for pain relief - especially for chronic pain. But the reality has shifted dramatically.
In 2021, over 80,000 people in the U.S. died from opioid overdoses. That’s not just a statistic - it’s a public health crisis. The CDC declared the opioid epidemic a public health emergency in 2017, and the guidelines haven’t softened since. The 2022 CDC Clinical Practice Guideline for Prescribing Opioids for Pain now says clearly: non-opioid therapy should be the preferred treatment for subacute and chronic pain.
Why? Because opioids don’t just relieve pain - they change how your brain works. Over time, your body builds tolerance, meaning you need higher doses to get the same effect. That increases the risk of dependence, addiction, and overdose. Even if you take them exactly as prescribed, long-term use can lead to serious health problems. One study of nearly 300,000 people found that taking opioids for 180 days or more over 3.5 years raised the risk of heart attack by more than 160%. Daily doses above 120 mg of morphine equivalent were linked to a 58% higher risk of heart attack compared to low doses or no opioids.
What Are Non-Opioid Pain Medications?
Non-opioid pain relievers are everything that doesn’t touch the opioid system. This includes:
- NSAIDs - like ibuprofen (Advil), naproxen (Aleve), and aspirin. These reduce inflammation and pain.
- Acetaminophen - Tylenol - which works on pain and fever without affecting inflammation.
- Newer non-opioid drugs - like Journavx, approved by the FDA in March 2024. This is the first new class of non-opioid painkiller for acute pain in decades.
Unlike opioids, these drugs don’t cause addiction. They don’t slow your breathing. They don’t create that euphoric high that leads to misuse. But they’re not without risks. Long-term NSAID use can irritate your stomach, raise blood pressure, or affect kidney function. Acetaminophen, if taken in excess, can cause serious liver damage. But these risks are manageable with proper dosing and monitoring - unlike opioid risks, which escalate quickly and unpredictably.
Do Opioids Work Better Than Non-Opioids?
This is the question most people ask: If opioids are stronger, why aren’t they better?
The answer comes from hard data. The SPACE trial, a major 12-month study published in JAMA in 2018, followed 240 patients with chronic back or knee/hip pain. Half were given opioids. Half got non-opioid meds like acetaminophen and NSAIDs. At the end of the year, there was no meaningful difference in how well they could function in daily life. In fact, the non-opioid group reported slightly better pain control - and far fewer side effects.
Another study, from the U.S. Department of Veterans Affairs, found opioids were not superior to non-opioid treatments for chronic pain - but came with significantly more side effects. Nausea, dizziness, constipation, and mental fog were far more common in the opioid group.
Even in kids, the data backs this up. A 2024 review in Pediatrics looked at five randomized trials comparing opioids like morphine and codeine to ibuprofen for post-surgery or fracture pain. No study showed opioids worked better. But the opioid groups had way more vomiting, drowsiness, and even cases of low oxygen levels. For children, the risks clearly outweigh any tiny benefit.
The New Kid on the Block: Journavx
In March 2024, the FDA approved Journavx - a completely new kind of non-opioid painkiller. It’s not an NSAID. It’s not acetaminophen. It’s a novel drug that targets a different pain pathway. It was tested in two large trials with 874 people recovering from surgery - like abdominoplasty and bunion removal.
Patients on Journavx had significantly less pain than those on placebo. And they didn’t need to reach for extra pain meds as often. Importantly, it didn’t cause the same respiratory depression or addiction risks as opioids. The FDA called it a "significant step" in reducing reliance on opioids for acute pain.
This isn’t just about one drug. It’s about a shift. The FDA is now actively funding research and offering grants to develop more non-opioid options. Why? Because the old model - reach for the opioid first - is outdated. And dangerous.
What Do Experts Really Say?
The American College of Physicians, the CDC, the VA, and even state medical boards like California’s are all on the same page now:
- Opioids have limited long-term benefits for chronic pain.
- The risks - addiction, overdose, heart problems - are real and well-documented.
- Non-opioid options are just as effective for most people.
- They’re safer, especially over time.
Dr. Roger Chou, lead author of the 2017 ACP guideline, put it plainly: "The evidence on long-term effectiveness is limited, and there are significant concerns about harms, including overdose and opioid use disorder."
That’s not a cautious opinion. That’s the consensus.
When Might Opioids Still Be Needed?
Let’s be clear: opioids aren’t evil. They have a place. For severe, short-term pain after major surgery, trauma, or cancer treatment, they can be life-changing. For some patients with advanced cancer or end-of-life care, they remain essential.
But for everyday chronic pain - lower back pain, osteoarthritis, headaches, fibromyalgia - they’re rarely the right first step. The guidelines now say: try everything else first. Physical therapy. Acupuncture. Exercise. Weight management. NSAIDs. Acetaminophen. Even cognitive behavioral therapy.
If those don’t work, and you’re still in pain, then - and only then - should opioids be considered. And even then, the dose should be the lowest possible, for the shortest time.
What Should You Do If You’re on Opioids?
If you’ve been on opioids for months or years, don’t panic. But do talk to your doctor. Ask:
- Is this still the best option for me?
- Have I been tested for signs of dependence or tolerance?
- Could I try cutting back or switching to a non-opioid?
- Am I getting regular check-ins on my pain and side effects?
Never stop opioids cold turkey. That can cause severe withdrawal. But with medical support, many people successfully reduce or stop opioids and find better long-term pain control with other tools.
Bottom Line: Safer Pain Relief Is Possible
The idea that stronger pain relief means stronger drugs is a myth. The data doesn’t support it. Non-opioid medications - from simple ibuprofen to brand-new drugs like Journavx - work just as well for most types of pain. And they don’t come with the risk of addiction, overdose, or heart damage.
Doctors aren’t just being cautious. They’re being smart. And patients are better off for it.
If you’re in pain, don’t assume opioids are the answer. Ask about alternatives. Ask about risks. Ask for a plan that keeps you safe - not just numb.


12 Comments
Destiny Annamaria
November 19, 2025 AT 15:47Finally someone says it loud and clear! I’ve been telling my aunt for years to ditch the oxycodone for her arthritis - she switched to naproxen and now she’s hiking again. No more zoning out at family dinners. 🙌
Jeremy Samuel
November 21, 2025 AT 05:10non opioid? more like non fun. if u wanna feel like a zombie try tylenol. opioids r the only thing that makes pain go away. ur body just needs to adjust. stop scaremongering.
Alyssa Torres
November 21, 2025 AT 11:32Y’all need to hear this: I was on opioids for 5 years after my surgery. Lost my job. Lost my kids’ trust. Started taking ibuprofen + physical therapy + acupuncture. I’m not ‘cured’ - but I’m alive. And I can hold my daughter again. This isn’t just medical advice - it’s a second chance. Please, if you’re struggling - reach out. You don’t have to suffer alone.
Kristi Bennardo
November 22, 2025 AT 19:56This article is dangerously naive. The FDA’s approval of Journavx was based on industry-funded trials with cherry-picked endpoints. The real data from the VA shows opioid tapering leads to increased suicide rates in chronic pain patients. You’re trading one crisis for another. This isn’t progress - it’s ideological overreach.
Dana Oralkhan
November 23, 2025 AT 23:52I’m a nurse who’s seen both sides. Opioids save lives in acute trauma - no doubt. But for chronic pain? I’ve watched patients turn into shadows of themselves. The real tragedy isn’t the pain - it’s how we’ve made people believe the only way out is through a pill that steals their soul. Non-opioid doesn’t mean ‘weaker’ - it means ‘wiser.’
Nicole Ziegler
November 24, 2025 AT 20:13me: takes ibuprofen like candy
my doctor: 😬
my liver: 🤖
Ravi boy
November 26, 2025 AT 08:49in india we use turmeric + hot water + yoga for back pain. no pills. no drama. just life. why do americans think every pain needs a chemical fix? 🤷♂️
Shiv Karan Singh
November 27, 2025 AT 08:21lol Journavx? sounds like a drug from a sci-fi movie. next they’ll patent ‘hope’ and sell it for $1200 a pill. opioids are the OG painkillers. if you can’t handle the side effects, maybe you’re not tough enough.
Aruna Urban Planner
November 27, 2025 AT 22:37The paradigm shift from pharmacological dominance to multimodal pain management reflects a broader epistemological evolution in clinical practice - moving from symptom suppression to systemic resilience. The pharmacokinetic profile of NSAIDs and acetaminophen, while not devoid of adverse events, presents a significantly lower risk-benefit ratio than mu-opioid receptor agonists in longitudinal cohorts. The emergence of non-opioid neuromodulatory agents like Journavx further supports this transition toward targeted, non-addictive analgesia.
Ron and Gill Day
November 28, 2025 AT 10:14Oh wow, another ‘non-opioid’ propaganda piece from the woke medical establishment. You people act like opioids are the devil. They’re just chemicals. If you can’t handle addiction, don’t take them. But don’t take away my right to choose what numbs my pain. I’ve been on them for 12 years - I’m not an addict, I’m a patient. And you’re the one being toxic.
Summer Joy
November 28, 2025 AT 13:39OMG I just read this and I’m CRYING 😭 I was on 120mg morphine a day for 3 years… my mom found me passed out on the bathroom floor last Christmas. I didn’t even know I was addicted until I saw the video. I switched to gabapentin and PT and now I can play with my dog again. I’m not ‘fixed’ - but I’m here. And I’m so grateful. If you’re reading this and still on opioids - please, please talk to someone. You’re not weak. You’re just human.
Bharat Alasandi
November 28, 2025 AT 15:22bro in india we use ginger tea and chai for everything. even for back pain. opioids? nah. we don’t need fancy drugs. just good sleep, good food, and no stress. also yoga. always yoga. 🙏