Imagine getting the right pill for your body-not just any generic version, but the one your genes actually respond to. That’s not science fiction anymore. Thanks to AI and pharmacogenomics, online pharmacies are starting to offer drug recommendations tailored to your DNA. This isn’t about fancy branding or marketing buzz. It’s about stopping dangerous side effects before they happen.
What Is Pharmacogenomics, Really?
Pharmacogenomics (PGx) is the study of how your genes affect the way your body handles drugs. Two people can take the same pill, but one gets relief while the other gets sick. Why? Because their genes process that drug differently. For example, about 20% of people have a variant in the CYP2D6 gene that makes them metabolize codeine too fast, turning it into dangerous levels of morphine. Others can’t turn it into morphine at all-so it doesn’t work. Without knowing your genes, you’re guessing.How AI Makes This Work at Scale
Interpreting genetic data used to take pharmacists 15 to 20 minutes per patient. Now, AI systems powered by models like GPT-4 can do it in under two minutes. These systems don’t guess. They pull from the Clinical Pharmacogenetics Implementation Consortium (CPIC) guidelines-the gold standard for gene-drug pairings-and cross-check your genetic variants against thousands of documented outcomes. A June 2024 study in JAMIA showed these AI tools correctly interpreted test results 89.7% of the time, outperforming human experts who averaged 82% accuracy. The real breakthrough? They explain it in plain language. Instead of a dense lab report full of terms like “rs1065852,” the AI says: “Your body breaks down this antidepressant too quickly. You’ll need a higher dose-or a different one.” Patients in testing reported 92% found these explanations clear. Doctors did too.How This Connects to Online Pharmacies
Most online pharmacies still just ship the same generic pills to everyone. But the ones leading the change are starting to ask: “Do you have a pharmacogenomic test result?” If you do, they match your genes to the drug they’re about to send. For common medications like warfarin, clopidogrel, or SSRIs, this isn’t optional anymore-it’s safer. Some platforms now integrate directly with genetic testing services like 23andMe or Invitae. Once you upload your raw DNA data (with consent), the pharmacy’s AI scans it for relevant variants and flags potential issues before processing your order. It doesn’t replace your doctor. It just gives your doctor-and your pharmacist-better intel.What This Means for Generic Drugs
Generics are cheaper, yes. But if your body doesn’t metabolize a generic version of a drug the same way as the brand, it might not work-or could harm you. AI helps solve that. It doesn’t care if the pill is branded or generic. It cares about the active ingredient and how your genes interact with it. For example, the generic version of clopidogrel (Plavix) needs to be activated by the CYP2C19 enzyme. If you’re a poor metabolizer (about 2-5% of people), that generic won’t prevent clots. AI spots this and recommends an alternative like ticagrelor, even if it’s more expensive. That’s not just smart-it’s life-saving.Where It’s Working-and Where It’s Not
The Mayo Clinic saw a 22% drop in adverse drug events in cardiac patients after using AI-guided PGx. At the University of Florida, doctors saved over 12 minutes per visit. That’s time they can spend talking to patients instead of decoding genetic reports. But it’s not perfect. In one case reported on Reddit, an AI system missed a critical CYP2D6 ultrarapid metabolizer status for codeine in a child. That’s a serious error. The system had been trained mostly on adult data. It didn’t have enough examples of pediatric cases. That’s why human oversight is still required. And here’s the catch: AI can’t read raw DNA. You still need a lab test. The AI only works with pre-processed results-like “CYP2C19*2/*2” or “SLCO1B1 c.521T>C.” If your test doesn’t cover those variants, the AI won’t know.Big Problems Holding It Back
First, data bias. Most genetic databases are 78% European ancestry. That means if you’re African, Asian, or Indigenous, the AI’s predictions are less reliable. A 2023 study in Cell Genomics found non-European patients were 3.5 times more likely to get incorrect drug recommendations. Second, integration. Most online pharmacies don’t talk to EHRs. They don’t know your full medication list. They don’t know if you’re taking statins, antifungals, or even grapefruit juice-all of which can interfere with gene-drug interactions. Without that context, the AI’s advice is incomplete. Third, regulation. Only one AI-PGx tool, GeneSight Psychotropic, has FDA clearance so far. Most others operate in a gray zone. If the AI recommends a drug that causes harm, who’s liable? The pharmacy? The testing company? The AI developer?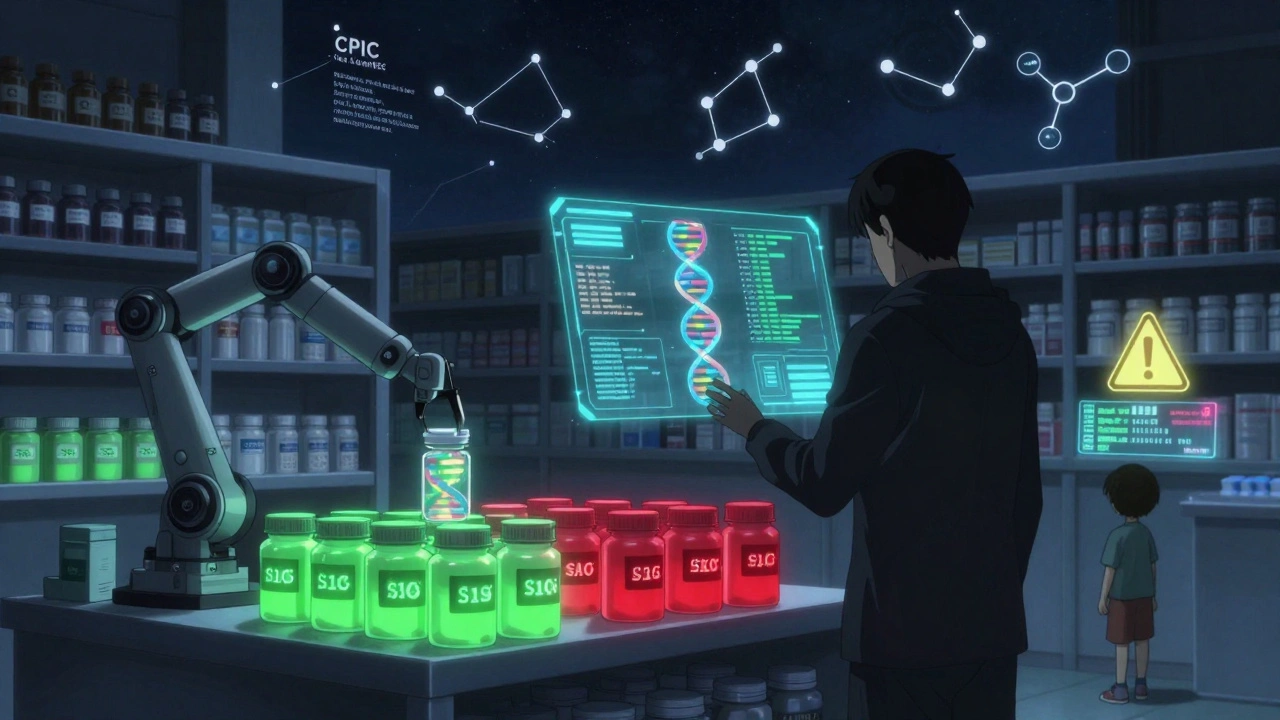
What You Can Do Today
You don’t need to wait for your pharmacy to catch up. Here’s how to get ahead:- Get a pharmacogenomic test from a reputable provider like Myriad Genetics, OneOme, or even 23andMe (which includes some PGx markers).
- Download your raw DNA data (usually a .txt file).
- Use a free tool like PharmGKB or GeneSight’s patient portal to upload it and see your results.
- Take that report to your doctor or pharmacist and ask: “Based on this, what medications should I avoid or use with caution?”
- When ordering generics online, share that report with the pharmacy’s support team. Some now accept it.
The Future Is Here-But It’s Not Automatic
By 2027, 45% of academic hospitals plan to combine PGx with polygenic risk scores to predict not just how you respond to a drug, but your overall risk for heart disease, diabetes, or depression-and tailor treatment accordingly. AI isn’t replacing doctors. It’s giving them superpowers. But those powers only work if the data is good, the system is transparent, and the patient is involved. If you’re using online pharmacies now, don’t just look for the lowest price. Ask: “Do you use genetic data to guide your recommendations?” If they say no, they’re still operating in the dark. And so are you.What’s Coming Next
DeepMind’s AlphaPGx, set to launch in 2025, will model how drugs bind to enzymes at the atomic level-something no human could visualize. The NIH just pledged $125 million over five years to build fairer, more accurate AI models. And CPIC updated its guidelines in May 2024 to include specific rules for AI use. This isn’t about replacing medicine. It’s about making it smarter, safer, and truly personal.Can AI really recommend the right generic drug based on my genes?
Yes-but only if your genetic test covers the right variants and the AI is trained on reliable data like CPIC guidelines. AI can tell you if a generic version of clopidogrel or warfarin will work for you, or if you need a different drug entirely. It doesn’t care if it’s branded or generic. It cares about your genes and how they interact with the active ingredient.
Do I need a prescription to use AI-powered pharmacogenomics?
You don’t need a prescription to get a genetic test, but you do need a doctor to interpret the results and prescribe medication. AI tools can help explain your test, but they can’t legally prescribe. Always share your results with a licensed provider before changing your meds.
Are online pharmacies already using this technology?
A few are-mostly large, tech-forward platforms tied to hospital systems or academic medical centers. Most still ship the same generic pills to everyone. But if you upload your PGx report, some will flag potential issues. Ask them directly: “Do you use genetic data to personalize drug recommendations?” If they don’t know what you’re talking about, they’re not using it yet.
Is my genetic data safe with an online pharmacy?
Only if they use HIPAA-compliant systems with end-to-end encryption and federated learning. Avoid pharmacies that ask you to upload raw DNA files directly to their website without clear privacy policies. Reputable platforms use secure portals tied to your EHR or partner with certified genetic labs. Never share your DNA with a site that doesn’t explain how it’s stored and protected.
What if I’m not of European descent? Will AI still work for me?
It’s less reliable. Most genetic databases are 78% European, meaning AI models are trained mostly on data from people who look like most of the researchers. If you’re African, Asian, Indigenous, or Latino, the AI may miss important variants or give incorrect advice. Always ask if the system was validated in diverse populations. If they can’t answer that, treat the recommendation with caution and confirm with a genetic counselor.
How much does a pharmacogenomic test cost?
Tests range from $100 to $500, depending on how many genes are analyzed. Some insurance plans cover it if ordered by a doctor for specific conditions like depression or heart disease. 23andMe’s Health + Ancestry service includes a few PGx markers for $199. For full coverage (CYP2D6, CYP2C19, SLCO1B1, etc.), companies like OneOme or Myriad offer clinical-grade panels-often covered if your doctor deems it medically necessary.
Can AI predict side effects I haven’t had yet?
Yes. It doesn’t wait for you to have a bad reaction. It looks at your genes and known drug interactions to predict risks before you take the medication. For example, if you’re a slow metabolizer of statins, AI can warn you that you’re at high risk for muscle damage-even if you’ve never had it before. That’s the power of prevention.
What’s the difference between AI pharmacogenomics and regular clinical decision support?
Traditional systems use simple rules: “If gene X, avoid drug Y.” They’re accurate about 78% of the time. AI systems use natural language understanding to interpret complex gene-drug interactions, explain them in plain terms, and even spot hidden patterns across multiple genes. They’re 89.7% accurate and can adapt as new evidence emerges. But they’re also more complex-and require human oversight to catch rare errors.



9 Comments
Marvin Gordon
December 5, 2025 AT 18:46This is wild. I got my 23andMe results last year and finally asked my pharmacist about it. They had no clue what I was talking about. Now I just send them the report and watch their face. Game changer.
Why are we still guessing with meds like it’s 1998?
Norene Fulwiler
December 6, 2025 AT 20:42As a Black woman who’s been misdiagnosed three times because doctors assumed my symptoms were ‘stress,’ this hits different.
I got tested after my cousin had a bad reaction to Plavix. The AI flagged me as a poor CYP2C19 metabolizer. Turned out I needed ticagrelor. No one else would’ve caught it. This tech saved my life.
But yeah, the data gap is real. My results were less reliable than my white coworkers’. We need more diverse training data. Not just for fairness-because lives depend on it.
Ada Maklagina
December 8, 2025 AT 06:50I uploaded my raw DNA to a pharmacy site and they asked for a doctor’s note. So I did. Then they said they don’t use AI. Just ‘manual checks.’ So I just pay extra for brand name now. Waste of time.
Harry Nguyen
December 9, 2025 AT 14:41So now we’re letting robots prescribe medicine because some Silicon Valley bro thinks he’s Hippocrates?
Next they’ll be using ChatGPT to decide if you get a kidney transplant. At least back in the day, a doctor looked you in the eye and said ‘you’re sick.’ Now it’s all algorithms and data points. We’re becoming code.
James Moore
December 11, 2025 AT 03:34Let’s not forget, the entire foundation of pharmacogenomics is built upon the assumption that genes are destiny-but epigenetics, environmental triggers, microbiome diversity, and even gut flora dynamics play a non-trivial, often dominant role in drug metabolism, which is why even the most ‘accurate’ AI systems, despite their 89.7% success rate, still fail catastrophically in cases where polygenic risk scores, lifestyle factors, and drug-drug interactions are not contextualized within a holistic physiological framework-so we’re not talking about a silver bullet, we’re talking about a very expensive, statistically biased, and ethically murky proxy for clinical judgment that, in the hands of untrained pharmacy clerks, could easily become a liability masquerading as innovation.
Kylee Gregory
December 12, 2025 AT 10:03I think the real win here isn’t the AI-it’s that patients are finally being asked to bring their own data to the table. For so long, medicine felt like a black box. Now, if you’ve got your report, you can walk in and say, ‘Here’s what my body says.’ That’s power.
And yeah, the system’s flawed. But flaws don’t mean we scrap it. They mean we fix it. Together.
Lucy Kavanagh
December 14, 2025 AT 09:34Wait… so you’re telling me Big Pharma and the government are secretly using this to track our DNA and then control which meds we get? Like, what if the AI is programmed to push certain drugs because the pharmaceutical companies paid for the training data?
I heard the NIH funding came from a company that owns 3 patents on gene-editing tech. Coincidence? I think not.
Also, my neighbor’s cousin’s dog got a test done and it said the dog was allergic to aspirin. So now the vet won’t give it pain meds. I think we’re being manipulated.
Chris Brown
December 16, 2025 AT 09:04It is profoundly irresponsible to entrust life-altering medical decisions to artificial intelligence systems that lack moral agency, legal accountability, and human intuition. The notion that a machine, trained on biased datasets and operated by corporate entities with profit motives, should dictate whether a patient receives warfarin or ticagrelor is not progress-it is a moral abdication of medical ethics.
And to those who say ‘just ask your doctor’-what if your doctor doesn’t understand the algorithm? What if they’re pressured to follow its recommendation? Who bears the burden of error? Not the AI. Not the corporation. Always the patient.
Stephanie Fiero
December 16, 2025 AT 18:46Okay so I just got my results from OneOme and I’m like… this is the most important thing I’ve ever done for my health. I’ve been on sertraline for 7 years and it barely worked. Turns out I’m a CYP2D6 ultra-rapid metabolizer. No wonder I felt nothing.
Switched to vortioxetine and my mood is stable for the first time in a decade. I’m crying right now. This isn’t sci-fi. This is real life.
And yes I know the data is skewed. And yes I know AI makes mistakes. But I’d rather take the risk with tech that’s 89% right than keep taking pills that don’t work and pretending it’s ‘just how I am.’
Go get tested. Don’t wait. Your body deserves better.