Medication-Induced Agranulocytosis Risk Calculator
Your Risk Assessment
Enter the medications you're currently taking to get personalized risk assessment and monitoring recommendations.
What Is Agranulocytosis and Why Should You Care?
Imagine waking up with a fever, a sore throat, and feeling like you’ve been hit by a truck-but no one can figure out why. You’ve taken your meds like always. No one’s been sick around you. No flu going around. Then your blood test comes back: your neutrophil count is below 100 per microliter. That’s agranulocytosis. It’s not common, but when it happens, it’s life-threatening. Your body has essentially lost its main defense against bacteria and fungi. Without neutrophils, even a minor cut or a cold can spiral into sepsis. And the scary part? In up to 70% of cases, it’s caused by medications you’re already taking.
Which Drugs Are Most Likely to Cause It?
Over 200 medications have been linked to agranulocytosis, but only a handful carry real risk. The biggest offender is clozapine, used for treatment-resistant schizophrenia. Even though it works better than any other antipsychotic, it carries a 0.77% chance of triggering agranulocytosis. That’s why the FDA requires weekly blood tests for the first six months. If your neutrophil count drops below 1,000/μL, you stop the drug. No exceptions.
Another high-risk group is antithyroid drugs. Propylthiouracil (PTU) causes agranulocytosis in about 0.36 out of every 1,000 patients per year. Methimazole is safer, but still risky. Then there are antibiotics like trimethoprim-sulfamethoxazole, which increases your risk 16 times compared to other antibiotics. Even common painkillers like dipyrone (banned in the U.S. but used elsewhere) have been tied to cases. On the flip side, ibuprofen and acetaminophen? Nearly no risk.
It’s not about the drug class alone-it’s about how your body reacts. Some people develop antibodies that attack their own neutrophils. Others have bone marrow that just shuts down production. That’s why two people on the same drug can have totally different outcomes.
How Do You Know If It’s Happening to You?
The symptoms are sneaky. They look like a bad cold or the flu: fever above 38.3°C, sore throat, mouth ulcers, chills, fatigue. But here’s the catch-most patients get dismissed. A 2022 survey found that 63% of people with drug-induced agranulocytosis had their symptoms written off as viral infections. By the time they get a proper blood test, it’s often too late.
There’s no warning sign before it hits. No rash, no itching. Just sudden, unexplained fever. If you’re on clozapine, PTU, or any high-risk drug, and you develop a fever, don’t wait. Go to the ER. Get a CBC with differential. If your ANC is below 500/μL, you’re in emergency territory. Delaying antibiotics increases your death risk from 5% to over 20%.

Monitoring Protocols: What Works and What Doesn’t
For clozapine, the system is strict: weekly blood tests for six months, then biweekly for another six, then monthly. It’s not optional. The Clozapine REMS program in the U.S. makes it mandatory. But here’s the problem-only 68% of doctors actually follow it. A 2020 study found that nearly a third of patients missed at least one test. And that’s where the danger hides.
Even with monitoring, 25% of clozapine-induced cases still happen. Why? Because the blood count can drop fast. One week it’s normal. The next, it’s below 100. That’s why new guidelines from the European Hematology Association now recommend acting when ANC falls below 1,000/μL-not 500. Catching it earlier saves lives.
For other high-risk drugs like PTU, monitoring is less standardized. Some doctors check blood every two weeks. Others wait a month. That inconsistency kills. The European Medicines Agency now classifies drugs into three risk tiers. Tier 1: clozapine, PTU, dipyrone-strict monitoring required. Tier 2: some anticonvulsants, certain chemotherapy agents-periodic checks. Tier 3: everything else-minimal risk. If your doctor doesn’t know your drug’s tier, ask.
New Tools Are Making Monitoring Easier
Waiting 48 hours for a lab result used to be the norm. Now, point-of-care devices like the Hemocue WBC DIFF can give you a neutrophil count in five minutes. It’s been cleared by the FDA since March 2022. In rural clinics or home settings, this changes everything. One trial showed adherence to monitoring jumped by 31% when patients could get results during their appointment.
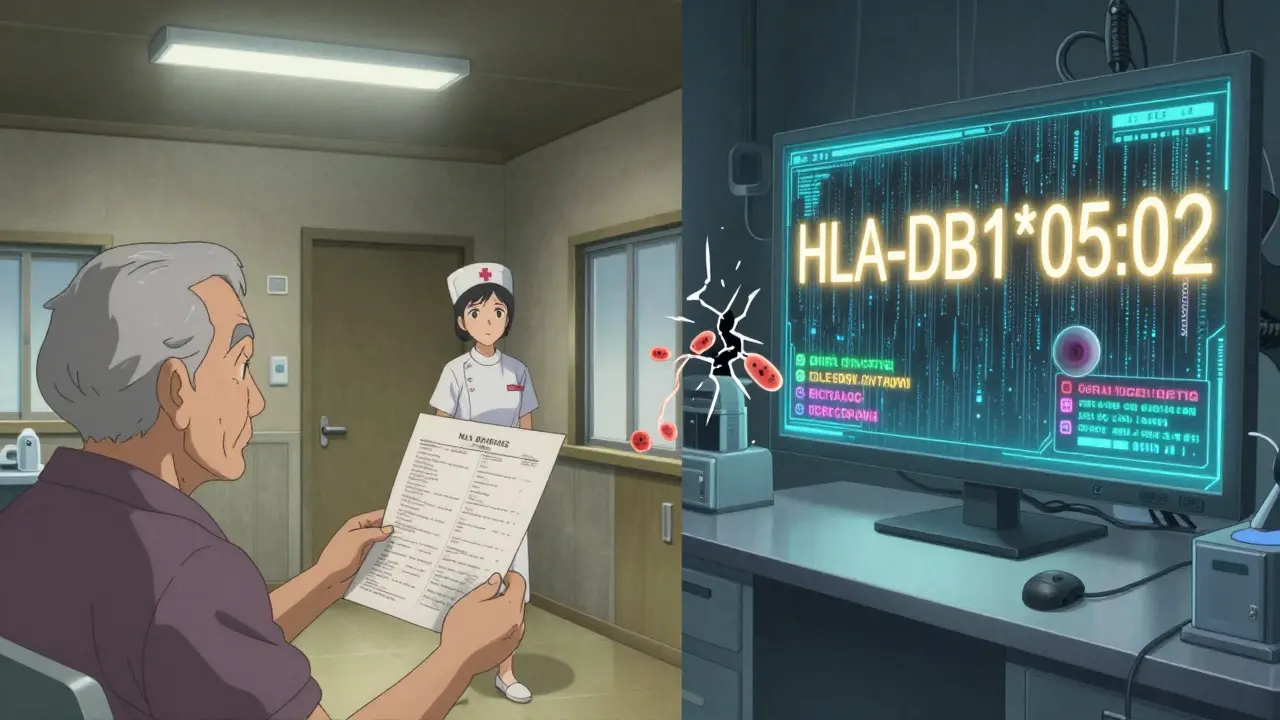
Even better, there’s now a genetic test. The HLA-DQB1*05:02 biomarker, approved by the FDA in early 2023, identifies people at 14 times higher risk of developing agranulocytosis from clozapine. If you test positive, your doctor might choose a different antipsychotic. This isn’t science fiction-it’s happening now in major hospitals.
AI is stepping in too. Electronic health records are being programmed to flag patients on high-risk drugs who haven’t had a blood test in 30 days. A 2022 study across 12 hospitals showed this cut missed cases by 47%. The future isn’t just more testing-it’s smarter, automated alerts.
What Happens After Diagnosis?
Step one: stop the drug. Immediately. No exceptions. Recovery usually takes one to three weeks. Your bone marrow wakes up. Neutrophils return. But if you keep taking the drug, you’re playing Russian roulette.
Step two: antibiotics. If you have a fever and low neutrophils, you need broad-spectrum antibiotics right away. Pseudomonas aeruginosa is the silent killer here. It’s in hospitals, in water pipes, even in soil. Your body can’t fight it without neutrophils. The IDSA guidelines say start antibiotics within an hour of fever onset. Delay even 30 minutes, and survival drops.
Step three: isolation. No crowds. No restaurants. No gym. No kids with colds. You’re immunocompromised. Even a handshake can be dangerous. Stay home. Wash hands. Wear a mask if you must go out. This isn’t caution-it’s survival.
Why This Matters More Than You Think
It’s not just about clozapine or PTU. It’s about awareness. Primary care doctors, ER staff, pharmacists-they all need to know the signs. A 2022 survey of 347 patients found that 73% blamed their delayed diagnosis on providers who didn’t link their symptoms to medication use.
And the disparities are real. Rural patients are 2.3 times more likely to die from this condition because they can’t get timely blood tests. In low-income countries, only 1 in 3 have proper monitoring. This isn’t just a medical issue-it’s a justice issue.
Pharmaceutical companies have paid out hundreds of millions in lawsuits over this. AstraZeneca settled 142 cases linked to Seroquel. The FDA has issued 27 safety alerts since 2010. But regulations alone won’t save lives. You need to know your meds. You need to ask questions. You need to demand testing if you’re on a high-risk drug.
What Should You Do Right Now?
- If you’re on clozapine, PTU, trimethoprim-sulfamethoxazole, or dipyrone-ask your doctor what your ANC monitoring schedule is.
- Know your last blood test result. Write it down. Don’t rely on memory.
- Set phone alarms for your next blood test. Miss one, and you’re at risk.
- If you develop a fever, sore throat, or mouth sores-go to the ER immediately. Say: ‘I’m on [drug name]. I think I might have agranulocytosis.’
- Carry a card in your wallet listing your high-risk medications and your doctor’s contact info.
This isn’t paranoia. It’s preparedness. Agranulocytosis is rare-but when it strikes, it strikes fast. And it doesn’t care if you’re young, healthy, or diligent. It only cares if you’re monitored.



15 Comments
Alex Flores Gomez
January 30, 2026 AT 07:17So let me get this straight-you’re telling me I can’t take a simple painkiller without my body turning on itself? And the FDA’s like, ‘eh, just get your blood drawn every week’? That’s not medicine, that’s a full-time job. I’m on clozapine and I’m already tired of being treated like a lab rat. Why isn’t there a pill that just... doesn’t do this?
Frank Declemij
January 31, 2026 AT 15:02The data on clozapine monitoring is clear. ANC below 1000/uL warrants immediate discontinuation. The 2020 study cited in the post showed a 41% increase in mortality when monitoring was missed. This isn't speculation. It's protocol.
Pawan Kumar
February 2, 2026 AT 09:44You know who really benefits from all this 'monitoring'? The pharmaceutical industry. Weekly blood tests? Mandatory labs? It's a revenue stream disguised as safety. The real cause of agranulocytosis? Toxic heavy metals in the water supply. The drugs are just scapegoats. They don't want you to know about the EPA's 2018 cover-up of cadmium levels in municipal systems. Ask yourself: who profits from fear?
DHARMAN CHELLANI
February 3, 2026 AT 10:15Bro, dipyrone’s banned in the US but everywhere else? People take it like candy. And now you’re telling me I gotta get blood work every week just because some pharma exec got rich off fear? Chill. My cousin took it for 12 years. No issues. Stop scaring people for clicks.
Robin Keith
February 5, 2026 AT 03:03It’s fascinating, really-how we’ve turned the human body into a statistical anomaly, a data point in a spreadsheet. We quantify life, reduce marrow to ANC values, and call it medicine. But what is a neutrophil, truly? Is it a cell? Or is it the last whisper of autonomy before the algorithm decides you’re no longer viable? We fear the drop in numbers, but we don’t fear the system that demands we fear it.
Sheryl Dhlamini
February 5, 2026 AT 19:58I had a friend on clozapine and she almost died because her doctor missed a test. She’s fine now but she carries a little card in her wallet like the post says. I cried when she showed me. Please, if you’re on one of these meds-DO NOT SKIP THE TEST. I’m begging you.
Doug Gray
February 6, 2026 AT 23:03The system is optimized for liability, not outcomes. AI flags missed tests? Cool. But who’s paying for the point-of-care devices? Who’s training the rural clinics? It’s all performative safety. We’re automating compassion while the real problem-access-is ignored. 🤷♂️
LOUIS YOUANES
February 7, 2026 AT 06:45I’ve been on PTU for three years. Got my blood drawn every two weeks like clockwork. My doctor’s office has a poster: 'Your Neutrophils Are Your Shield.' I don’t care if it’s corporate fluff-it works. I’m alive. Don’t be lazy. Get tested.
paul walker
February 7, 2026 AT 13:40This post saved my life. I was ignoring my sore throat because I thought it was just stress. Then I remembered the part about fever + clozapine = ER. Went in. ANC was 380. They started antibiotics right away. I’m still here. If you’re reading this-don’t wait. Seriously.
ryan Sifontes
February 7, 2026 AT 15:29They say it’s rare. But if you’re the one it happens to? It’s 100%. And the fact that rural folks die 2.3x more? That’s not a medical failure. That’s systemic neglect. They don’t care if you’re in Nowhere, Montana. Your life is a cost-benefit analysis.
Laura Arnal
February 8, 2026 AT 15:02You guys are doing AMAZING by even reading this. Seriously. Knowledge is power. If you're on a high-risk med, you’re already ahead of 90% of people. Keep asking questions. Keep tracking. You got this 💪❤️
Jasneet Minhas
February 8, 2026 AT 23:37Ah yes, the classic 'get your blood tested' solution. Meanwhile, in India, most people pay out of pocket for a CBC. Imagine telling someone earning $3/day to drop $15 for a test every week. The 'tier system' sounds nice on paper. In reality? It’s a luxury. 🤡
Eli In
February 10, 2026 AT 00:35I’m from a country where antibiotics are sold over the counter. We don’t have labs. We don’t have AI alerts. We have grandmas who know when someone is 'off.' Maybe the real answer isn’t more tech-it’s community. Someone noticing you’re not yourself. That’s the original monitoring system.
Megan Brooks
February 11, 2026 AT 19:58The ethical imperative here is clear: autonomy requires information. If a patient is not informed of the risk profile of their medication, informed consent is a fiction. The onus is not solely on the individual to 'demand testing'-it is on the medical system to provide it proactively, without requiring the patient to become an advocate for their own survival.
Ryan Pagan
February 12, 2026 AT 02:26Let’s be real-this isn’t just about blood counts. It’s about being seen. When you’re on clozapine, you’re not just a patient. You’re a walking red flag. People look at you weird. Nurses sigh when you say you need a CBC. But here’s the thing: your life isn’t a footnote in a drug leaflet. You’re not a risk. You’re a person. And you deserve better than being treated like a ticking bomb. Don’t let them make you feel guilty for needing help.