Benzodiazepine Interaction Checker
Check Your Medication Combinations
Enter your medications to see if there are dangerous interactions with benzodiazepines.
No interaction detected
No dangerous combinations identified
When you're drowning in anxiety, a pill that works in minutes can feel like a lifeline. Benzodiazepines-like Xanax, Valium, or Ativan-are fast, effective, and widely prescribed. But here’s the part most people don’t talk about: benzodiazepines aren’t just risky on their own. Their real danger comes from what happens when they mix with other drugs you might be taking-painkillers, sleep aids, even alcohol.
How Benzodiazepines Actually Work
Benzodiazepines don’t just calm you down-they slow down your brain. They boost GABA, the main calming neurotransmitter in your nervous system. That’s why they work so fast: within 30 to 60 minutes, your racing heart slows, your muscles relax, and the panic starts to fade. For someone having a panic attack or going through severe withdrawal, that speed can be lifesaving.
But this same mechanism is why they’re dangerous. Slowing the brain too much means slowing your breathing. And when you combine that with other drugs that do the same thing, the effect isn’t just added-it’s multiplied.
The Deadly Mix: Benzodiazepines and Opioids
If you’re taking an opioid for chronic pain-oxycodone, hydrocodone, fentanyl-and your doctor also prescribes Xanax for anxiety, you’re in a high-risk zone. The FDA found that between 2011 and 2016, 75% of all benzodiazepine-related overdose deaths involved opioids. That’s not a coincidence. It’s a chemical collision.
Both drug classes depress the central nervous system. Together, they can shut down your breathing without warning. A 2018 CDC study showed that people taking both drugs together had a 15-fold higher risk of fatal overdose than those taking opioids alone. And it’s not just street drugs-this happens in homes where prescriptions are taken exactly as directed.
One patient on Reddit described it plainly: “I was on oxycodone for back pain and Xanax for panic attacks. One night, I stopped breathing in my sleep. I woke up in the ER with a breathing tube.” That’s not rare. Emergency rooms across the U.S. see this every week.
Alcohol: The Silent Killer
Alcohol is the most common drug people mix with benzodiazepines-and the one they least expect to be dangerous. A glass of wine at dinner. A beer after work. It seems harmless. But alcohol and benzodiazepines both hit the same brain receptors. Together, they can cause extreme drowsiness, confusion, loss of coordination, and respiratory failure.
Healthgrades analyzed over 1,200 patient reviews of benzodiazepines. Nearly 30% of negative reviews mentioned dangerous reactions after drinking. One user wrote: “I had a glass of wine with my Ativan and couldn’t stand up. My husband had to call 911.”
The FDA now requires all benzodiazepine prescriptions to include a Boxed Warning-its strongest safety alert-about combining them with alcohol. Yet, a 2022 survey by the Anxiety and Depression Association of America found that 32% of benzodiazepine users were prescribed the drug while also using alcohol regularly. Many didn’t realize it was a risk.
Other Dangerous Interactions
It’s not just opioids and alcohol. Many common medications can turn a benzodiazepine into a hazard.
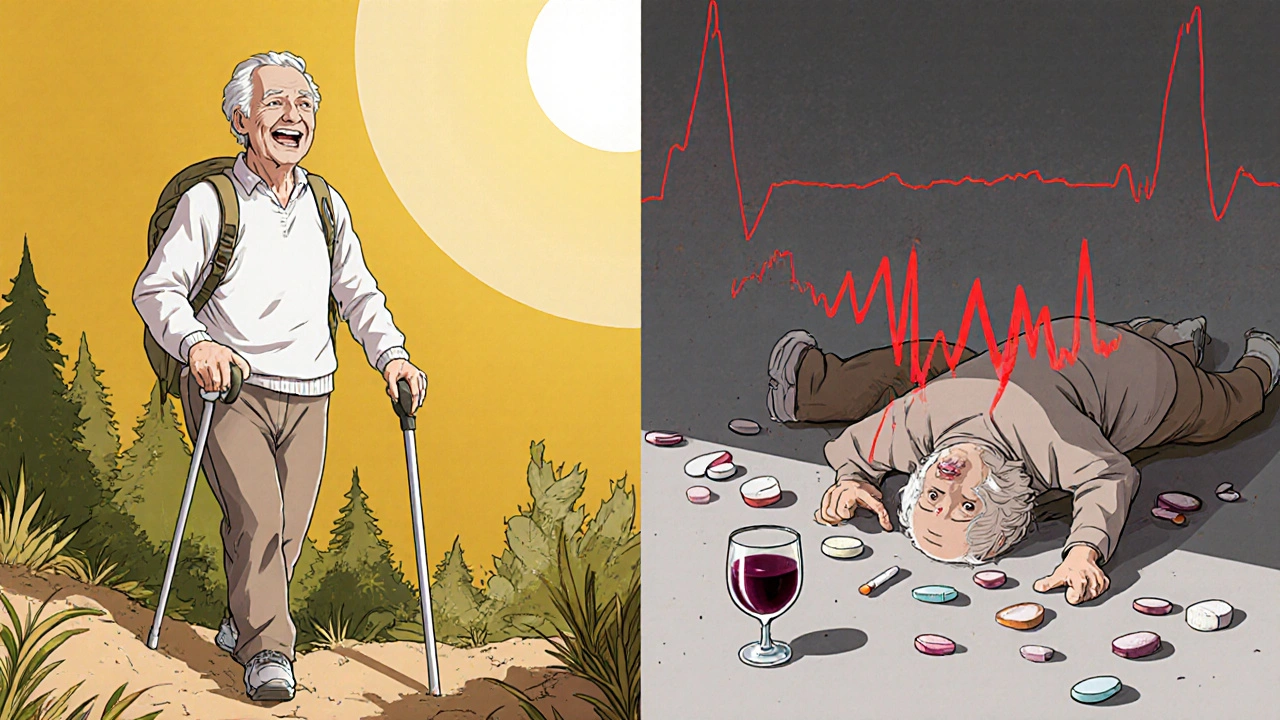
- Sleep aids (Z-drugs) like Ambien or Lunesta: These work similarly to benzodiazepines. Mixing them increases dizziness, memory loss, and risk of falls-especially dangerous for older adults.
- Antidepressants like SSRIs: While SSRIs themselves are safer for long-term anxiety, combining them with benzodiazepines can cause excessive sedation. It’s not usually deadly, but it can leave you too groggy to drive or work.
- Muscle relaxants like cyclobenzaprine: These add to CNS depression. People on these combinations often report feeling “drunk without drinking.”
- Antihistamines like diphenhydramine (Benadryl): Found in sleep aids and cold medicines, they’re often overlooked. But they’re CNS depressants too.
Older adults are especially vulnerable. The American Geriatrics Society says benzodiazepines should be avoided entirely in people over 65. Why? They increase the risk of falls by 50%. When combined with other sedating drugs, that risk triples. A simple stumble can lead to a hip fracture-and for seniors, that often means the end of independent living.
Why Doctors Still Prescribe Them
It’s not because they’re ignorant. It’s because they’re stuck.
SSRIs like sertraline or escitalopram are the first-line treatment for anxiety. But they take 4 to 6 weeks to work. For someone in acute distress-unable to sleep, trembling, avoiding social situations-that’s too long. Benzodiazepines offer immediate relief. So doctors prescribe them, often for just a few weeks.
But here’s the problem: many patients don’t get the follow-up. They keep taking it. The FDA says about 40% of people who use benzodiazepines for more than six months develop physical dependence. Quitting cold turkey can trigger seizures, hallucinations, or rebound anxiety worse than before.
And when patients come back saying, “I can’t stop,” doctors may feel pressured to keep prescribing-especially if they’re not trained in tapering protocols.
What Safe Use Actually Looks Like
Safe use isn’t about never taking benzodiazepines. It’s about using them the right way.
- Short-term only. Two to four weeks max. That’s the guideline from the American Psychiatric Association.
- No opioids. If you’re on pain meds, ask your doctor for alternatives to benzodiazepines. Buspirone or cognitive behavioral therapy (CBT) are safer options.
- No alcohol. Even one drink can be risky. If you drink, don’t take it. If you take it, don’t drink.
- Know your meds. Check every pill you take-even over-the-counter ones. Many cold and sleep meds contain hidden depressants.
- Taper slowly. If you’ve been on it longer than a month, don’t quit on your own. Work with your doctor. Long-acting benzos like diazepam are easier to taper than short-acting ones like alprazolam.
One patient on Drugs.com wrote: “My doctor prescribed Ativan for two weeks after surgery. He told me not to mix it with alcohol or pain pills. I followed the rules. It worked perfectly.” That’s how it’s supposed to be.
What’s Changing in 2025
Prescriptions for benzodiazepines have dropped from 13.1% of U.S. adults in 2013 to just 10.8% in 2021. Why? Awareness. Regulation. Better alternatives.
Since 2020, the FDA has required updated warnings on every benzodiazepine bottle. Medicare now requires special approval before doctors can prescribe benzodiazepines with opioids. Many states have added alerts in prescription monitoring systems that flag dangerous combinations before they’re filled.
And more patients are asking questions. The rise of non-drug treatments-CBT, mindfulness, exercise-is shifting the landscape. SSRIs are now prescribed for 68% of new anxiety cases. Benzodiazepines? Only 22%.
The message is clear: benzodiazepines aren’t gone. But they’re no longer the go-to. They’re a last resort, used carefully, with eyes wide open to the risks.
What You Should Do Right Now
If you’re on a benzodiazepine:
- Check every medication you take-prescription, OTC, herbal. Look for anything that causes drowsiness.
- Ask your doctor: “Am I on any other drugs that could interact with this?”
- If you drink alcohol, tell your doctor. Don’t assume it’s fine.
- If you’ve been on it longer than a month, ask about tapering. Don’t wait until you feel dependent.
- If you’re on opioids, ask if there’s a safer alternative for your anxiety.
If you’re not on one but considering it:
- Ask about SSRIs or therapy first. They’re safer for long-term use.
- If you need something fast, ask for a short-term script with a clear end date.
- Never take someone else’s prescription. Even if they have the same diagnosis.
The goal isn’t to scare you. It’s to make sure you know the real stakes. Benzodiazepines can help-but only if you treat them like the powerful, dangerous drugs they are.
Can you die from mixing Xanax and alcohol?
Yes. Mixing Xanax (alprazolam) and alcohol can cause severe respiratory depression, loss of consciousness, coma, or death. Both substances depress the central nervous system, and together they can shut down your breathing. This combination is responsible for thousands of emergency room visits and hundreds of deaths each year in the U.S. The FDA requires all benzodiazepine packaging to include a Boxed Warning against alcohol use.
How long should you take benzodiazepines for anxiety?
Guidelines from the American Psychiatric Association and the FDA recommend benzodiazepines for no longer than 2 to 4 weeks. They’re meant for short-term relief during acute anxiety episodes, not long-term management. Using them longer increases the risk of dependence, tolerance, and severe withdrawal symptoms. For ongoing anxiety, SSRIs or therapy are safer, more effective options.
Are there safer alternatives to benzodiazepines for anxiety?
Yes. SSRIs like sertraline (Zoloft) and escitalopram (Lexapro) are first-line treatments for anxiety disorders and have no abuse potential. SNRIs like venlafaxine are also effective. Non-drug options like cognitive behavioral therapy (CBT) have been shown to be as effective as medication long-term, with no side effects. Buspirone is another non-addictive medication that works for generalized anxiety, though it takes weeks to help.
What are the signs of benzodiazepine dependence?
Signs include needing higher doses to get the same effect, feeling anxious or irritable when the drug wears off, experiencing insomnia or tremors without it, and being unable to stop even when you want to. Physical dependence can develop after just a few weeks of daily use. Withdrawal can include seizures, hallucinations, and rebound anxiety worse than before. Never stop cold turkey-always taper under medical supervision.
Why are benzodiazepines still prescribed if they’re so risky?
They work quickly. For someone having a panic attack, a benzodiazepine can bring relief in minutes-something SSRIs can’t do. In emergencies, like severe agitation or alcohol withdrawal, they’re still essential. The problem isn’t their use-it’s their overuse and long-term use without proper monitoring. Doctors are now being trained to use them only as a bridge to safer, long-term treatments.
Can you get off benzodiazepines safely?
Yes, but it requires a slow, supervised taper. Stopping suddenly can be dangerous. For short-acting benzos like Xanax, reductions of 5-10% every 1-2 weeks are typical. Long-acting ones like diazepam allow for slightly faster tapers. Many people need support from a psychiatrist or addiction specialist. Withdrawal can last weeks or months, but with the right plan, full recovery is possible.
Final Thoughts
Benzodiazepines aren’t evil drugs. They’ve helped millions. But they’re not harmless either. The biggest threat isn’t the pill itself-it’s the quiet, unnoticed combination with other substances. The safest approach isn’t fear. It’s awareness. Know what you’re taking. Talk to your doctor. Ask questions. And never assume a prescription is automatically safe.



12 Comments
JAY OKE
November 25, 2025 AT 21:42Been on Xanax for 3 years. Didn't realize how much I was mixing it with wine until my buddy called me out. One night I couldn't walk straight. Scared the hell out of me. Cut back to weekends only. Still take it, but now I know the line.
Stephen Adeyanju
November 26, 2025 AT 01:07YALL THINK THIS IS BAD WAIT TIL YOU SEE WHAT HAPPENS WHEN YOU MIX BENZOS WITH OPIATES AND SLEEP MEDS AND ALCOHOL AND ALSO TAKE MELATONIN BECAUSE YOU THINK ITS HARMLESS LOL
Sanjay Menon
November 27, 2025 AT 21:47The real tragedy isn't the pharmacology-it's the cultural normalization of chemical sedation as a substitute for existential reckoning. We've outsourced our anxiety to pharmaceutical corporations while abandoning the ancient practices of breath, movement, and community. Benzodiazepines are merely the symptom of a civilization that has forgotten how to be still.
Cynthia Springer
November 29, 2025 AT 01:37I'm curious-how many people actually read the Boxed Warning on the bottle? Or do they just glance at the dosage and assume it's fine? I've seen friends take it with Tylenol PM and say 'it's just a little something to help me sleep.' No one thinks it's a problem until it is.
Rachel Whip
November 30, 2025 AT 16:29For anyone on SSRIs and considering benzos: talk to your pharmacist. They're the unsung heroes who catch these interactions before the doctor even prescribes. I had a patient come in on sertraline and alprazolam-she didn't know the combo made her feel like a zombie. We switched her to buspirone. She’s been off benzos for 18 months now and says she feels more alive than she has in years.
Ali Miller
December 1, 2025 AT 15:10THE GOVERNMENT IS USING BENZOS TO KEEP THE POPULATION DULL AND SUBMISSIVE. THEY KNOW IF YOU'RE TOO AWAKE YOU'LL ASK QUESTIONS. THAT'S WHY THEY PUSH THEM WITH OPIOIDS-TO MAKE YOU TOO GROGGY TO PROTEST. THE FDA'S 'WARNING' IS JUST A SMOKE SCREEN. THEY WANT YOU TO THINK YOU'RE SAFE WHILE THEY CONTROL YOUR MIND.
mohit passi
December 2, 2025 AT 21:32Bro, I was in India last year and saw my uncle take Ativan for insomnia. His doctor said 'only one, never with alcohol.' He followed it. No drama. No addiction. Just a quiet life. Maybe the problem isn't the drug-it's how we treat our minds here. We want quick fixes. But peace? That takes time 🙏
Marissa Coratti
December 3, 2025 AT 23:04It's profoundly concerning that our healthcare system prioritizes immediate symptom suppression over long-term psychological resilience. The overprescription of benzodiazepines reflects a systemic failure to invest in evidence-based psychotherapeutic interventions, such as cognitive behavioral therapy, which have demonstrated superior durability and zero physiological dependence. We must redirect funding, training, and policy toward sustainable mental health infrastructure-not chemical band-aids.
Ezequiel adrian
December 5, 2025 AT 21:19My cousin died from mixing Xanax and codeine cough syrup. He was 22. His mom didn't even know it was dangerous. She thought it was just a cold. Now she can't leave the house. If you're reading this and you're on benzos? Stop pretending you're safe. You're not. Talk to someone before it's too late.
Joe bailey
December 7, 2025 AT 20:33Man I used to take Ativan with a beer after work like it was nothing. Then I got dizzy driving home one night and nearly hit a tree. Scared me straight. Now I drink water, do yoga, and call my mate. Life’s better without the chemical crutch 🙌
Amanda Wong
December 7, 2025 AT 23:59This post is pure fearmongering. Benzodiazepines have saved my life during panic attacks. You people act like they're heroin. SSRIs made me numb for two years. I'd rather be alert and anxious than a walking zombie. If you can't handle responsibility, don't blame the medication.
james thomas
December 8, 2025 AT 22:42They’re hiding the truth. The pharmaceutical companies made billions off this. They funded the studies that said ‘it’s safe.’ They paid off the doctors. And now they’re pretending they care? The real danger isn’t the drug-it’s the system that lets them sell it like candy. Wake up. This isn’t medicine. It’s a controlled addiction.