High blood pressure doesn’t come with warning signs. You might feel fine, but your arteries are under constant strain. Left unchecked, it silently increases your risk of heart attack, stroke, and kidney failure. That’s why millions of people take blood pressure medications every day - not because they feel sick, but because they know the numbers on the monitor matter more than how they feel.
What Are the Main Types of Blood Pressure Medications?
There are ten main classes of blood pressure drugs, but most people start with just one or two. The four most commonly prescribed are diuretics, calcium channel blockers, ACE inhibitors, and ARBs. These are chosen because they’ve been proven over decades to reduce serious complications.
Diuretics, often called water pills, help your kidneys flush out extra salt and water. This lowers the volume of blood flowing through your vessels, which reduces pressure. Hydrochlorothiazide is the most common one. It’s cheap, effective, and often the first drug doctors reach for, especially for people over 65 or those with heart failure.
Calcium channel blockers like amlodipine work by relaxing the muscles in your blood vessel walls. This makes your arteries wider, so blood flows more easily. They’re especially helpful for Black patients and older adults, who often respond better to these than to ACE inhibitors. Amlodipine is the #2 most prescribed blood pressure med in the U.S. - and for good reason.
ACE inhibitors - such as lisinopril - block a chemical that narrows blood vessels. By stopping this process, they help vessels stay relaxed. They’re also used for people with diabetes or kidney disease because they protect the kidneys. But there’s a catch: about 1 in 5 people develop a persistent dry cough. It’s not dangerous, but it’s annoying enough that many stop taking them.
ARBs, like losartan, do almost the same thing as ACE inhibitors but block the effect at a different point. The big advantage? They rarely cause the dry cough. If you can’t tolerate lisinopril, your doctor will likely switch you to losartan. They’re equally good at protecting the heart and kidneys.
Beta-blockers - such as metoprolol - slow your heart rate and reduce the force of each beat. They’re not usually first-line anymore, unless you’ve had a heart attack or have heart failure. They’re also used for anxiety-related high blood pressure, since they calm the nervous system.
What Are the Most Common Side Effects?
Side effects are why so many people stop taking their blood pressure meds. You might feel fine at first, then start noticing dizziness, swelling in your ankles, or needing to pee all the time. It’s not laziness - it’s biology.
With diuretics, you’ll likely need to go to the bathroom more often, especially at first. You might also get low potassium, which can cause muscle cramps or irregular heartbeat. Some people notice their gout flares up. That’s because diuretics raise uric acid levels.
Calcium channel blockers like amlodipine can cause swollen ankles, flushing, headaches, and sometimes a fast heartbeat. Gingival hyperplasia - overgrown gums - is rare but real. If you notice your gums are puffier than usual, tell your dentist. It’s not just poor hygiene.
ACE inhibitors bring the dry cough. It’s not an allergy. It’s a chemical side effect caused by buildup of a substance called bradykinin. It usually starts within weeks. If it’s bad, you won’t get used to it. You’ll need to switch.
ARBs don’t cause coughs, but they can raise potassium levels. That’s dangerous if you have kidney disease. Your doctor will check your blood regularly, especially in the first few months.
Beta-blockers can make you tired, cold, or give you trouble sleeping. For diabetics, they can hide the warning signs of low blood sugar - like shaking or a fast heartbeat. That’s risky. If you have diabetes, you need to check your glucose more often.
Some meds - like alpha-blockers or methyldopa - are used less often because they cause dizziness when standing up. That’s called orthostatic hypotension. It’s a big fall risk for older adults. If you feel lightheaded when you stand, sit down. Don’t rush.
What Makes a Medication Safe for You?
Safety isn’t about the drug. It’s about you - your age, your other health problems, your lifestyle, even your race.
If you’re Black, guidelines say to start with a diuretic or calcium channel blocker. ACE inhibitors and ARBs tend to work less well in this group. That’s not a flaw in the drugs - it’s how your body processes them. Your doctor should know this.
If you have diabetes, ACE inhibitors or ARBs are the top choice. They don’t just lower blood pressure - they slow kidney damage. That’s huge. One study showed they cut the risk of kidney failure by 30% in diabetic patients.
If you’ve had a heart attack, beta-blockers are lifesavers. They cut the chance of another one by nearly half. They’re not just for lowering pressure - they’re for protecting your heart muscle.
If you’re pregnant, most blood pressure drugs are off-limits. ACE inhibitors and ARBs can cause serious birth defects. Methyldopa and labetalol are the go-to options. They’ve been used safely for decades.
Older adults need lower starting doses. Your body processes drugs slower. A dose that’s fine for a 40-year-old might knock an 80-year-old off their feet. Start low. Go slow.

What Happens When Medications Don’t Work Alone?
Most people need more than one pill. About 70% of people with high blood pressure require two or more drugs to reach their target. That’s normal. It’s not failure.
Current guidelines say if your blood pressure is 140/90 or higher, you should start with two medications from different classes right away. No more waiting months to add the second one.
The most common combos are:
- Diuretic + ACE inhibitor
- Diuretic + calcium channel blocker
- ACE inhibitor + calcium channel blocker
- ARB + diuretic
Some pills even come in one tablet - like lisinopril-hydrochlorothiazide or amlodipine-valsartan. Fewer pills means better adherence. That’s the goal.
Don’t mix ACE inhibitors and ARBs together. It sounds logical - two drugs that do the same thing - but it’s dangerous. Studies show it raises your risk of kidney failure and high potassium without lowering blood pressure any better.
Also avoid NSAIDs like ibuprofen or naproxen. They can cancel out your blood pressure meds and hurt your kidneys. If you need pain relief, talk to your doctor. Acetaminophen is usually safer.
How Do You Know If It’s Working?
High blood pressure has no symptoms. So you can’t rely on how you feel. You need to check your numbers.
Your doctor will want to see you in 2-4 weeks after starting a new med or changing a dose. Then every 3-6 months once things are stable. Blood tests for potassium, sodium, and kidney function are routine - especially if you’re on ACE inhibitors, ARBs, or diuretics.
Home monitoring helps. A simple cuff at home gives you more accurate data than one reading at the clinic. Many people have “white coat hypertension” - their pressure spikes just because they’re at the doctor’s office.
Track your readings. Write them down. Bring them to your next visit. It helps your doctor decide if you need a higher dose, a different drug, or an extra pill.
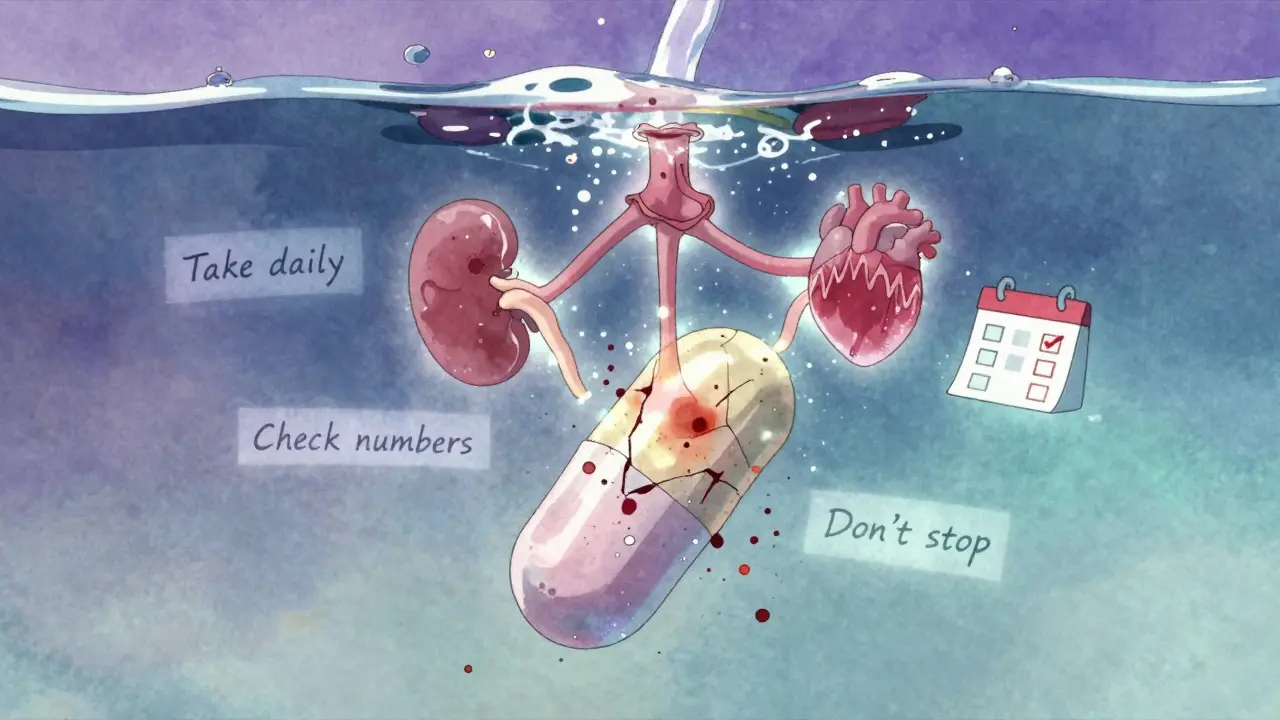
Why Do So Many People Stop Taking Their Meds?
Half of all people stop taking their blood pressure meds within a year. Why?
- They don’t feel sick, so they think they don’t need it.
- The side effects are annoying - peeing all night, swollen ankles, dry cough.
- They forget. Taking four pills a day is hard.
- They’re scared of long-term use.
But stopping suddenly is dangerous. Your pressure can spike back up - sometimes dangerously high. That’s when strokes happen.
Here’s what works: simplify. Ask your doctor if you can switch to a once-daily combo pill. Use a pill organizer. Set phone reminders. Talk to your pharmacist - they can help you build a routine.
And remember: you’re not taking these pills because you’re sick. You’re taking them so you don’t get sick.
What’s New in Blood Pressure Treatment?
Research is moving fast. The SPRINT trial showed that lowering systolic pressure to below 120 mmHg - instead of the old target of 140 - cuts heart attacks and strokes in high-risk people. But it also increases side effects like dizziness and kidney issues. So it’s only for people with existing heart disease or kidney problems.
Doctors are also looking at genetics. Some people respond better to certain drugs based on their DNA. A blood test might soon tell you if you’re more likely to benefit from a beta-blocker or a calcium channel blocker. It’s not routine yet, but it’s coming.
Digital tools are helping too. Apps that remind you to take your pill and log your blood pressure have been shown to improve adherence by 15-20%. That’s huge. If you’re struggling, ask your doctor about one.
And while new drugs are being tested - like endothelin blockers - they’re still for rare, resistant cases. For most people, the old standbys - diuretics, calcium channel blockers, ACE inhibitors, ARBs - still work best.
What Should You Do Next?
If you’re on blood pressure meds:
- Don’t stop. Even if you feel fine.
- Take them at the same time every day.
- Know your numbers - check them at home if you can.
- Tell your doctor about side effects. Don’t suffer in silence.
- Ask if you can switch to a combo pill.
If you’ve been told you need meds but haven’t started:
- Don’t wait. High blood pressure doesn’t get better on its own.
- Ask your doctor which class is right for you - based on your age, race, and other conditions.
- Start with one. You can add more later if needed.
Managing high blood pressure isn’t about perfection. It’s about consistency. One pill, every day. That’s how you protect your heart, your brain, your kidneys. And that’s how you stay healthy - even if you don’t feel a thing.


15 Comments
innocent massawe
January 2, 2026 AT 14:06This is so helpful. I never knew why my uncle's gums were swollen until now. 🙏
Tru Vista
January 2, 2026 AT 22:15Diuretics cause gout? Lmao. My doc never mentioned that. Guess I'll just stop taking them. 😴
Kerry Howarth
January 4, 2026 AT 00:20Consistency > perfection. One pill, every day. That's the mantra.
Sarah Little
January 4, 2026 AT 19:03The pharmacokinetic variability across ethnic groups is a critical consideration in precision hypertension management, especially given the renin-angiotensin-aldosterone system (RAAS) polymorphisms that modulate ACE inhibitor efficacy in African ancestry populations. Failure to account for this leads to suboptimal outcomes.
Haley Parizo
January 5, 2026 AT 01:15They're hiding the truth. These drugs are designed to keep you dependent. The cough? The swelling? The potassium spikes? All part of the pharmaceutical playbook. You think they care if you live or die? They care about your subscription.
Neela Sharma
January 5, 2026 AT 08:12In India, we call this 'dabba dard' - the silent thief of life. One pill, one day, one heartbeat saved. No drama. Just duty.
Ian Detrick
January 6, 2026 AT 15:05I love how this breaks down the science without the fluff. People think meds are a crutch. Nah. They're armor. Wear it proudly.
Angela Fisher
January 6, 2026 AT 15:30I read somewhere that the FDA approves these drugs because they're funded by Big Pharma. The cough? It's not just bradykinin - it's a cover-up. They know ACE inhibitors make people quit, so they push ARBs. But ARBs? They're just the same poison in a new bottle. And don't get me started on combo pills - they're just a trap to make you think you're doing less work. I stopped all meds. Now I drink lemon water and meditate. My BP is better than my doctor's.
Ian Ring
January 7, 2026 AT 15:48I appreciate the clarity here. Especially the note about NSAIDs - I didn't realize ibuprofen could sabotage my meds. Thank you. 🙏
veronica guillen giles
January 8, 2026 AT 18:30Oh, so now we're supposed to believe that 'black people don't respond to ACE inhibitors'? That's not biology - that's lazy medicine. You think your genes are the problem? No. It's your doctor's laziness. You don't test. You don't adjust. You just slap on a diuretic and call it a day. Pathetic.
Brittany Wallace
January 8, 2026 AT 19:50This post made me cry. Not because I'm scared - because I finally feel seen. I've been on three meds for six years. No one ever explained why. Thank you.
Joy F
January 9, 2026 AT 04:50You know what's really dangerous? The belief that you can 'fix' high blood pressure with a pill. It's a symptom. A symptom of stress, of capitalism, of not having time to breathe. We're treating the symptom, not the soul. Your arteries aren't clogged with salt - they're clogged with grief. And no pill can dissolve that. But maybe... maybe a walk. Maybe silence. Maybe a moment where you stop being a patient and start being a person.
Shanahan Crowell
January 10, 2026 AT 09:56You're not weak for needing meds. You're smart. You're choosing your future over your fear. Keep going. One pill. One day. One life saved.
Shruti Badhwar
January 12, 2026 AT 01:15The combination of ARB with diuretic remains the most evidence-based regimen for patients with metabolic syndrome. It is imperative to monitor serum creatinine and potassium levels during initiation and titration phases.
Tiffany Channell
January 12, 2026 AT 21:31Wow. So the 'old standbys' are still the best? How original. And you wonder why people don't trust doctors. You just listed five drugs that each have a 1 in 5 chance of wrecking your life - and you call it 'science'. Meanwhile, the real solution - diet, sleep, stress - gets zero airtime. You're not educating. You're gaslighting.