When a drug causes a severe reaction, the instinct is clear: never take anything like it again. But here’s the problem - not every reaction means you need to avoid an entire class of medications. Too often, patients are told to steer clear of whole families of drugs based on a single bad experience, leaving them with fewer treatment options, longer hospital stays, or even dangerous delays in care. The truth is, severe drug reaction doesn’t always equal lifelong avoidance of a whole drug family. Knowing when to avoid a class - and when you might still be safe - can change your health outcomes forever.
What Counts as a Severe Drug Reaction?
Not all bad reactions are created equal. The FDA defines a severe adverse drug reaction as one that’s life-threatening, requires hospitalization, causes permanent disability, or leads to a birth defect. These aren’t just side effects like nausea or dizziness. They’re events that demand immediate attention and careful follow-up. Examples include:- Anaphylaxis - sudden swelling, trouble breathing, drop in blood pressure
- Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN) - life-threatening skin peeling
- DRESS syndrome - rash, fever, swollen lymph nodes, and organ damage
- Severe liver or kidney injury directly tied to the drug
These reactions aren’t common, but when they happen, they’re serious. About 1.3 million emergency room visits in the U.S. each year are due to drug reactions, and nearly 350,000 result in hospital admission. The key question isn’t just whether you had a bad reaction - it’s what kind of reaction it was.
Allergic vs. Non-Allergic Reactions: The Big Difference
Many people think any bad reaction means they’re "allergic." But in reality, 80-90% of reported drug reactions aren’t true allergies at all. They’re side effects, not immune responses. True allergic reactions involve your immune system. They usually happen quickly - within minutes to a few hours - and include symptoms like hives, swelling of the throat, wheezing, or anaphylaxis. These are often IgE-mediated and carry a high risk of recurrence. If you’ve had anaphylaxis to penicillin, avoiding all beta-lactam antibiotics is usually necessary. Non-allergic reactions are different. They’re predictable based on how the drug works in your body. For example:- NSAIDs like ibuprofen can cause stomach bleeding - that’s a pharmacological effect, not an allergy
- Statins might cause muscle pain - this isn’t an immune response
- Amoxicillin can cause a non-itchy rash in kids - often harmless and not a reason to avoid all penicillins
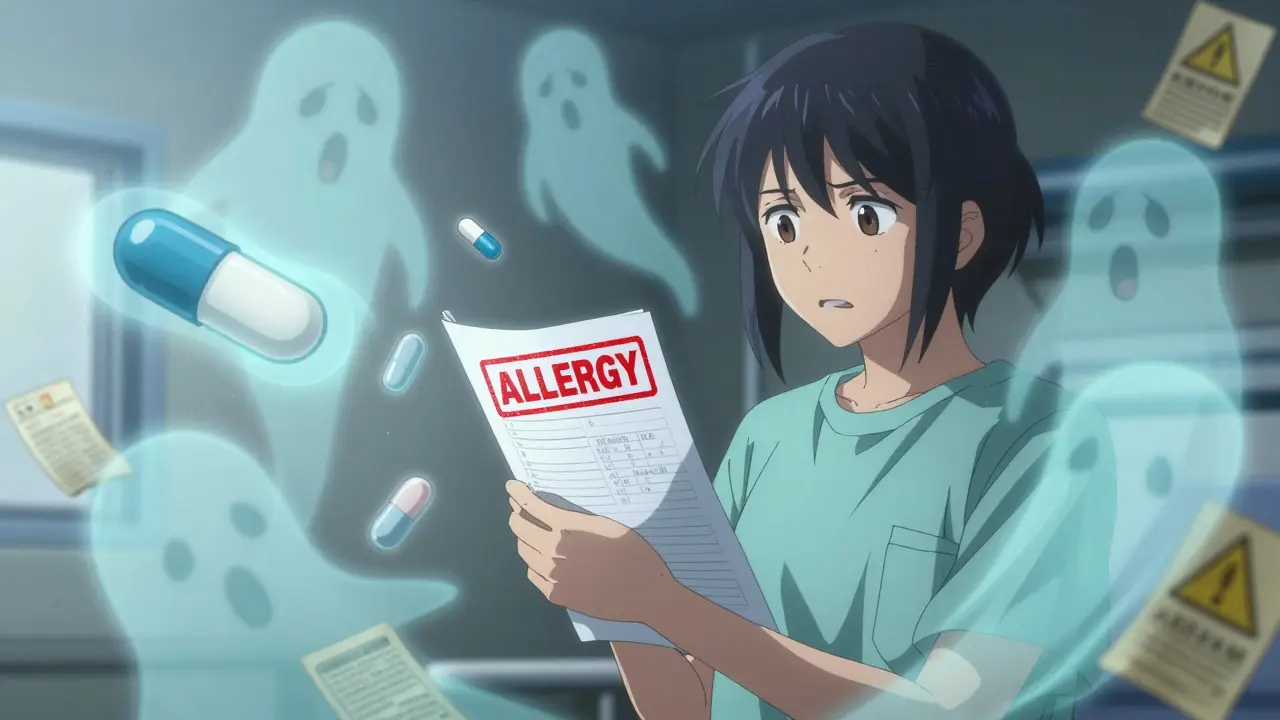
Here’s the catch: if you had a mild rash from amoxicillin as a child, you probably don’t need to avoid all penicillins for life. Yet, many patients are still labeled "penicillin allergic" decades later - even though studies show 95% of those labels are wrong. That’s not just inconvenient; it’s dangerous. Patients with false allergy labels are more likely to get broader-spectrum antibiotics, which increase the risk of resistant infections like C. diff.
Drug Families with High Cross-Reactivity Risks
Some drug classes have well-documented cross-reactivity. Avoiding the whole family makes sense here - but only if the reaction was truly immune-mediated. Beta-lactams (penicillins, cephalosporins, carbapenems): Cross-reactivity between penicillins and cephalosporins is only 0.5-6.5%, depending on the specific drugs. If you had anaphylaxis to amoxicillin, you might still safely take cefdinir or ceftriaxone after proper testing. But if you had TEN from a cephalosporin, avoid all beta-lactams. Sulfa drugs (Bactrim, sulfasalazine): True sulfa allergy is rare. Most people react to the antibiotic part (sulfamethoxazole), not the sulfur molecule itself. Drugs like furosemide (a water pill) or celecoxib (a painkiller) contain sulfur but aren’t chemically related to sulfa antibiotics. Yet, many patients are denied these entirely after a reaction to Bactrim. That’s unnecessary - and limits treatment options for conditions like arthritis or heart failure. NSAIDs (ibuprofen, naproxen, aspirin): Cross-reactivity depends on the type of reaction. If you have aspirin-exacerbated respiratory disease (AERD), you’ll likely react to most NSAIDs - up to 70% of patients do. But if you only got a stomach ache from ibuprofen, switching to celecoxib (a COX-2 inhibitor) is often safe. Anticonvulsants (carbamazepine, phenytoin): These are linked to SCARs like SJS and DRESS. If you had a severe skin reaction to one, avoid the entire class. Genetic testing for HLA-B*15:02 can identify high-risk patients before starting carbamazepine - especially in people of Asian descent.
When Avoidance Is Non-Negotiable
Some reactions are so dangerous that avoiding the entire drug family is the only safe choice. Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are medical emergencies. TEN alone has a 30-50% mortality rate. If you’ve had either, you must avoid the drug class that caused it - and often, all closely related drugs. The European Medicines Agency found that 95% of TEN cases come from just six drug classes: sulfa antibiotics, anticonvulsants, allopurinol, NSAIDs, nevirapine, and corticosteroids. Once you’ve had TEN from one of these, the risk of recurrence is too high. DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms) can damage your liver, kidneys, or heart months after the reaction starts. Even if you feel fine now, restarting the drug can trigger a deadly relapse. Avoid the entire class. Anaphylaxis from any drug requires strict avoidance - but only if it’s confirmed as IgE-mediated. Many people assume they had anaphylaxis when they actually had a vasovagal reaction (fainting from pain or anxiety). Proper testing can tell the difference.How to Know If You Really Need to Avoid the Whole Family
Don’t rely on old chart notes or what a nurse told you ten years ago. Here’s how to get it right:- Document the exact reaction - What symptoms? When did they start? Did you need epinephrine or ICU care? Vague terms like "allergic to penicillin" are useless.
- Ask for allergy testing - Skin tests and blood tests (like ImmunoCap) can confirm IgE-mediated allergies. For penicillin, these tests are 90% accurate. If negative, you can likely take penicillin safely.
- Consider a drug challenge - Under medical supervision, you can be given a small, controlled dose of the drug to test your reaction. Success rates for beta-lactam challenges are 70-85% in low-risk patients.
- Check your genetic risk - For drugs like abacavir (used for HIV), testing for HLA-B*57:01 can prevent a deadly reaction. This is now standard care.
- Update your records - If testing shows you’re not allergic, make sure your EHR is corrected. Many hospitals now have "de-labeling" programs to fix outdated allergy entries.
Only 28% of electronic health records contain enough detail to guide safe prescribing. That’s why so many patients get denied safe medications. Your reaction history matters - but only if it’s documented correctly.
What Happens When You Avoid Too Much?
Over-avoidance isn’t harmless. It leads to:- Delayed treatment - Patients with false penicillin labels wait an average of 3.2 days longer for the right antibiotic
- More side effects - Doctors turn to broader antibiotics like vancomycin or fluoroquinolones, which increase the risk of C. diff, kidney damage, or tendon rupture
- Higher costs - Alternative drugs are often more expensive and require more monitoring
- Worse outcomes - Studies show patients with unverified penicillin allergies have 50% higher rates of hospital readmission
One patient on HealthUnlocked shared that after being labeled "penicillin allergic" for 20 years, a simple skin test let her take amoxicillin for a sinus infection - no reaction, no problem. She’s now off unnecessary antibiotics and feels healthier than she has in decades.
What You Can Do Right Now
If you’ve had a severe reaction:- Don’t assume you’re allergic to the whole class
- Ask your doctor: "Was this a true allergy, or a side effect?"
- Request a referral to an allergist - especially if you’ve been avoiding multiple drugs
- Get your allergy label verified with testing
- Update your medical records and wear a medical alert bracelet if you truly have a high-risk allergy
Medication avoidance isn’t about fear - it’s about precision. You deserve the right treatment, not the safest guess. With better testing and smarter protocols, you can avoid dangerous drugs without giving up safe ones.
If I had a rash from penicillin as a child, do I need to avoid all antibiotics forever?
Not necessarily. A non-itchy, non-life-threatening rash from penicillin in childhood is often a non-allergic reaction - especially if it appeared days after starting the drug. Up to 95% of people labeled "penicillin allergic" based on childhood rashes can safely take penicillin or other beta-lactams after proper evaluation. Skin testing or a supervised oral challenge can confirm whether you’re truly allergic.
Can I take sulfa-based painkillers if I’m allergic to Bactrim?
Possibly. Bactrim (sulfamethoxazole-trimethoprim) is a sulfonamide antibiotic. Painkillers like celecoxib (Celebrex) or furosemide (Lasix) contain a sulfur atom but are not chemically similar to sulfa antibiotics. True cross-reactivity between sulfa antibiotics and non-antibiotic sulfonamides is less than 10%. Most reactions to Bactrim are immune-mediated and don’t extend to these other drugs. Still, talk to your doctor - and never self-prescribe.
What’s the difference between anaphylaxis and a panic attack after taking a drug?
Anaphylaxis involves physical changes: low blood pressure, swelling of the airway, hives, wheezing, and often vomiting or diarrhea. It’s caused by immune system chemicals like histamine. A panic attack causes rapid heartbeat, sweating, and dizziness - but no swelling, rash, or drop in blood pressure. If you’ve had both, an allergist can help distinguish them using clinical history and, if needed, blood tests for tryptase (a marker released during anaphylaxis).
Why do some doctors still avoid entire drug classes after one bad reaction?
Many doctors rely on outdated chart notes or fear liability. If a patient had a severe reaction, avoiding the whole class seems safer - even if the reaction wasn’t allergic. But this approach is changing. Hospitals with formal allergy de-labeling programs have reduced inappropriate antibiotic use by up to 30%. The American College of Allergy, Asthma, and Immunology now strongly recommends testing and re-evaluation instead of blanket avoidance.
Is there a blood test to confirm a drug allergy?
Yes - but only for some drugs. For penicillin, ImmunoCap Specific IgE blood tests are 89% accurate. For other drugs like vancomycin or cephalosporins, testing is less reliable. Skin testing is often more sensitive for penicillin. For non-IgE reactions (like DRESS or SJS), no blood test exists - diagnosis is based on clinical symptoms and timing. Genetic tests are available for specific drugs like abacavir and carbamazepine.


13 Comments
Monte Pareek
December 21, 2025 AT 06:03Let me cut through the noise - if you got a rash from penicillin at 7 and now you’re 45 and your doctor still won’t prescribe amoxicillin, you’re not allergic you’re just stuck in a 1980s chart note. 95% of these labels are wrong. Get tested. Stop letting outdated fear kill your treatment options. This isn’t just inconvenient - it’s killing people with C. diff because doctors are too lazy to look past the word "allergy".
holly Sinclair
December 21, 2025 AT 11:58It’s fascinating how medicine still operates on myth rather than mechanism. We’ve mapped the human genome but we still treat drug reactions like medieval curses - "you touched this, you’re cursed forever." The truth is far more nuanced. A non-itchy rash in childhood? Likely a viral exanthem mimicking a drug reaction. Anaphylaxis? That’s different - that’s your immune system screaming. But we don’t distinguish. We just blanket ban. And in doing so, we weaponize caution into ignorance. We’re not protecting people - we’re just making them sicker with worse, broader antibiotics. The system isn’t broken - it’s just asleep.
Vicki Belcher
December 21, 2025 AT 14:10This is so important!! 🙌 I had the "penicillin allergy" label for 15 years until I finally got tested - turns out I was fine!! Took amoxicillin for a sinus infection and felt great 😊 No hives, no panic, just relief. Why do we still let old notes dictate our health? Please, if you’ve been told "avoid all beta-lactams," ask for a referral to an allergist. It’s life-changing. 🌟
Alex Curran
December 21, 2025 AT 20:08I work in rural Australia and see this all the time. Patients come in with 10+ drugs they can't take because of a childhood rash. No testing no follow up just a note in the system. We end up using vancomycin for a simple UTI because they're "allergic" to amoxicillin. It's not just bad medicine it's lazy medicine. Get tested if you can.
Lynsey Tyson
December 22, 2025 AT 03:42I think this is such a gentle reminder that we don’t have to live in fear of every past mistake. My mom was told she was allergic to sulfa after a mild rash - turned out she just had a sunburn and was on Bactrim. She avoided all pain meds for 20 years because of it. When she finally got tested, she could take celecoxib without issue. It’s not about being reckless - it’s about being accurate.
Edington Renwick
December 22, 2025 AT 05:18Everyone’s acting like this is some groundbreaking revelation. Newsflash: doctors have been overcautious since the 1950s. It’s not ignorance - it’s liability. If you die because I gave you penicillin after you said "I think I’m allergic," I lose my license. If you die because I didn’t give you penicillin and gave you vancomycin instead? I get a pat on the back. So yeah - I’ll keep avoiding the whole class. You want precision? Pay for an allergist. Don’t expect your ER doc to risk their career.
Aboobakar Muhammedali
December 23, 2025 AT 08:42in india we dont have access to allergy testing for most people. so we just go with what the doctor says. but i remember my cousin got a rash from amoxicillin as a kid and now she cant take any antibiotic. she got pneumonia last year and had to wait 4 days because no one would prescribe penicillin. she almost died. this is not just a us problem. its a global problem. we need better education not just testing.
Laura Hamill
December 24, 2025 AT 19:04Big Pharma loves this. They want you afraid of penicillin so you’ll buy their expensive new antibiotics. They don’t want you getting tested because then you’d use cheap generics again. That’s why your doctor won’t listen. That’s why your chart says "allergic" even when you never had a reaction. This is all about profit. The system is rigged. Wake up.
Dikshita Mehta
December 25, 2025 AT 03:52This is one of the most clinically accurate summaries I’ve seen on this topic. The distinction between allergic and non-allergic reactions is critical, and the data on cross-reactivity in beta-lactams and sulfa drugs is well cited. I’ve personally seen patients denied celecoxib after a Bactrim reaction - and it’s medically unjustified. The real barrier isn’t science - it’s documentation. EHRs need structured fields for reaction type, timing, and severity. Until then, we’re flying blind.
pascal pantel
December 26, 2025 AT 06:42Let’s be real - this entire post is a glorified marketing piece for allergy testing clinics. You’re telling people to get tested, but you’re not acknowledging that 80% of these tests are false negatives or inconclusive. And then you push "drug challenges" - which carry real risk. What you’re really advocating is shifting liability from the prescriber to the patient. If you want precision medicine, start by fixing the reimbursement model. Until then, blanket avoidance is the only rational choice for any provider who wants to keep their malpractice insurance.
Gloria Parraz
December 27, 2025 AT 00:55I’m a nurse and I’ve seen this play out too many times. A patient comes in with a 20-year-old note saying "penicillin allergy" - no details, no symptoms, no date. We give them ceftriaxone anyway after checking the guidelines. No reaction. They cry. They say they’ve been avoiding so many meds for so long they forgot what it felt like to be treated properly. This isn’t just about antibiotics - it’s about dignity. You deserve to be heard. You deserve to be tested. Don’t let a piece of paper decide your health.
Sahil jassy
December 28, 2025 AT 06:59my dad had a rash from sulfa in 1990 now he cant take any water pill or painkiller with sulfur. he has heart failure and they gave him lasix last year he had a reaction but it was just itching. no swelling no breathing issue. but now he cant take any diuretic. this is ridiculous. we need better info not more fear. 🙏
Kathryn Featherstone
December 29, 2025 AT 08:43Thank you for writing this. I’m a pharmacist and I’ve spent years trying to convince doctors to de-label patients. One woman came in with 17 drugs she couldn’t take - all because of a childhood rash. We did a supervised challenge with amoxicillin. She took it. No reaction. She cried. Said she hadn’t slept through the night in 15 years because of sinus infections she couldn’t treat. This isn’t just medicine. It’s freedom.