Walking down the grocery store aisle should be simple. But for many people over 50, it becomes a slow, painful march - legs heavy, tingling, burning - forcing them to stop, bend forward, and lean on a shopping cart just to catch their breath. This isn’t just old age. It’s neurogenic claudication, the most common symptom of lumbar spinal stenosis. And if you’ve been told it’s just circulation problems, you might be missing the real cause - and the right treatment.
What Exactly Is Neurogenic Claudication?
Neurogenic claudication isn’t a disease. It’s a signal. Your nerves are being squeezed. When the spinal canal in your lower back narrows - usually from years of wear and tear - the nerves that run down to your legs get compressed. This isn’t like a muscle cramp. It’s nerve pain. And it doesn’t go away with rest alone. You feel it when you stand or walk. The pain starts in your lower back, then shoots into one or both buttocks, thighs, and calves. It feels like your legs are full of lead. Numbness, tingling, or weakness follows. The only thing that helps? Bending forward. Leaning on a walker. Pushing a shopping cart. Sitting down. Even crouching over a kitchen counter gives relief. This is the famous shopping cart sign. About 7 out of 10 people with this condition report it. Why does bending forward help? Because it opens up the space in your spinal canal. When you stand straight, the canal gets tighter. Bend forward, and the space opens up again - like releasing pressure on a pinched hose. That’s why cycling often feels easier than walking. You’re already leaning forward.How Is It Different From Vascular Claudication?
This is where things get critical. Many doctors, even experienced ones, mistake neurogenic claudication for vascular claudication - a problem with blood flow, not nerves. But the treatments are completely different. Getting this wrong means wasting months on the wrong care. Vascular claudication comes from blocked arteries. Your leg muscles don’t get enough oxygen when you walk. The pain is deep, crampy, and goes away after a few minutes of rest - no matter if you’re standing, sitting, or lying down. You might also have cold feet, weak pulses in your ankles, or sores that won’t heal. Neurogenic claudication? Your pulses are normal. Your feet feel warm. The pain only lifts when you bend forward. It’s not about blood. It’s about space. A simple test: Walk until your legs hurt. Stop. Sit down. If the pain doesn’t fade after two minutes, you’re probably not dealing with vascular issues. Now bend forward - if the pain disappears within 30 seconds, you’re likely looking at spinal stenosis.How Do Doctors Diagnose It?
There’s no single test that confirms neurogenic claudication. Diagnosis is built on clues. A good doctor will ask:- Do your legs hurt when you walk or stand?
- Do you feel better when you sit or lean forward?
- Do you use a shopping cart or walker to help you walk farther?
- Do you feel weakness or numbness in your legs while walking?
What Happens If You Ignore It?
Left untreated, neurogenic claudication doesn’t just stay the same. It gets worse. You’ll walk less. You’ll stop going out. You’ll avoid stairs. You might start using a cane or walker just to get around the house. Over time, you could lose muscle strength in your legs. Some people develop foot drop - where their toes drag when they walk. That’s not normal aging. That’s nerve damage. The good news? Progress is usually slow. Most people have symptoms for years before they become disabling. That gives you time to act - before it’s too late.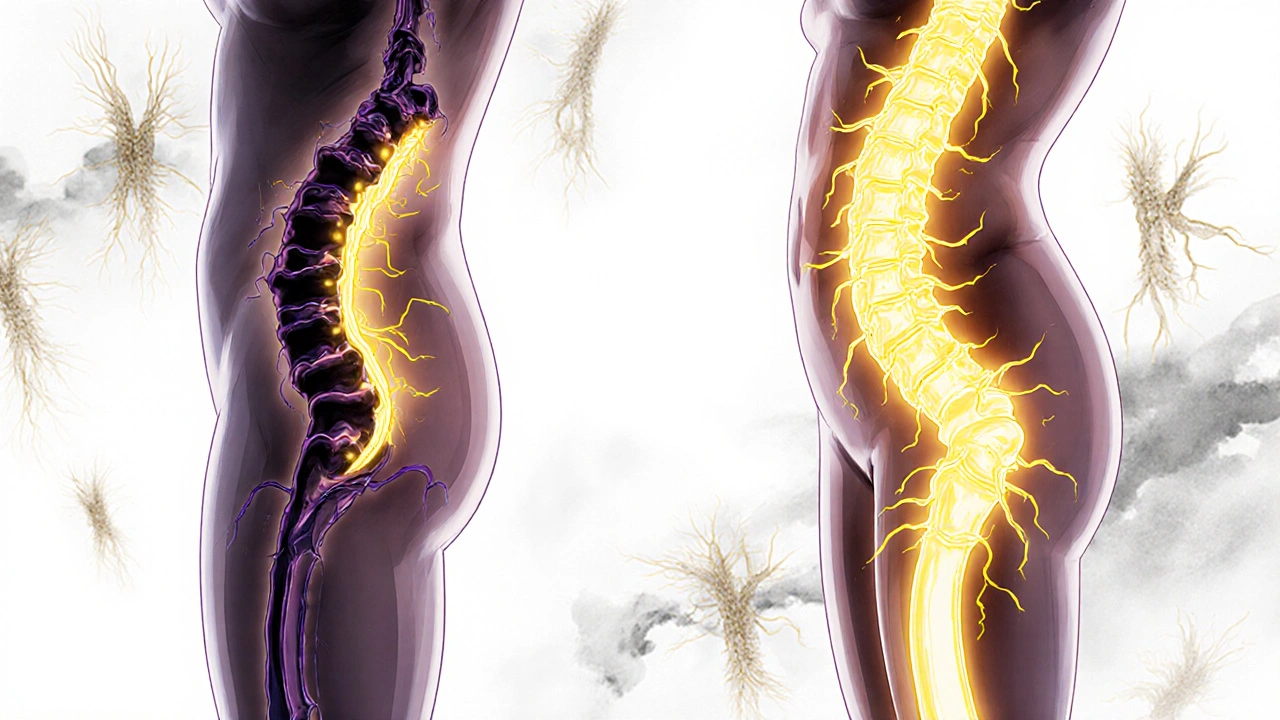
First-Line Treatment: Conservative Care
Before you think about surgery, try the basics. For most people in the early stages, non-surgical care works well. About 8 out of 10 patients see real improvement with conservative methods.- Exercise: Focus on flexion-based movements. Walk with a walker or shopping cart. Do pelvic tilts. Try seated forward bends. Avoid extension exercises like back extensions or standing toe touches. Physical therapy usually lasts 6 to 8 weeks. Consistency matters more than intensity.
- Medication: Over-the-counter pain relievers like acetaminophen or NSAIDs (ibuprofen, naproxen) help with inflammation and discomfort. If pain is severe, short-term nerve pain meds like gabapentin or pregabalin may be prescribed.
- Posture training: Learn to walk with a slight forward lean. Use a cane or walker to help you maintain that position. Many patients report walking 30% farther just by changing how they stand.
- Weight management: Extra weight adds pressure on your spine. Losing even 5-10 pounds can make a noticeable difference.
When Injections Might Help
If pain persists after 3 to 6 months of exercise and meds, epidural steroid injections may be considered. These shots deliver anti-inflammatory medicine directly around the compressed nerves. About half to 7 out of 10 people get relief - but it’s temporary. Lasts anywhere from a few weeks to 6 months. It’s not a cure. It’s a bridge - to help you stick with physical therapy or delay surgery. Some clinics offer nerve blocks or radiofrequency ablation, but these are less commonly used for neurogenic claudication. They work better for back pain, not leg symptoms.Surgery: When It’s Time
Surgery isn’t the end of the road - it’s often the beginning of regaining your life. If you’ve tried conservative care for 6 months and you’re still in pain, losing strength, or avoiding activities you love, it’s time to talk to a spine surgeon. The most common procedure is a laminectomy - removing part of the bone that’s pressing on the nerves. Sometimes a laminotomy (removing only a small piece) or a minimally invasive approach is enough. Newer devices like the Superion interspinous spacer, FDA-approved in early 2023, open the space without removing bone. Studies show 78% of patients report satisfaction two years later. Success rates? About 70 to 80% of carefully selected patients experience major improvement in leg pain and walking ability after surgery. Recovery takes 6 to 12 weeks. Most people can walk without assistance within a month. But surgery isn’t for everyone. If you have other serious health problems - heart disease, diabetes, or poor circulation - your risks go up. Your doctor will weigh the benefits against your overall health.
What Patients Really Say
On patient forums, the same stories keep coming up:- “I thought I had poor circulation. My doctor checked my pulses and said I was fine. Then he asked if I leaned forward. I said yes. He said, ‘That’s your answer.’”
- “I used to walk my dog every day. After six months of pain, I stopped. I thought I was just getting old. Turns out, I just needed to bend forward - and then get surgery.”
- “It took three doctors before someone asked about the shopping cart. I cried. I felt like I’d been heard.”
What’s Next for Treatment?
Research is moving fast. The International Spine Study Group is finalizing a new diagnostic algorithm expected in late 2024 - designed to help doctors match symptoms to imaging more accurately. Minimally invasive techniques are becoming more common, with a 35% rise in these procedures between 2018 and 2022. And with the global population over 65 expected to double by 2050, spinal stenosis will only become more common. The goal isn’t just to treat it - it’s to treat it earlier, better, and with less risk.What You Can Do Today
If you’re over 50 and walking has become painful:- Keep a symptom journal. Note when the pain starts, how long it lasts, and what helps.
- Try walking with a shopping cart or walker. If it helps, that’s a strong clue.
- Ask your doctor: “Could this be spinal stenosis?” Don’t let them dismiss it as just aging.
- Start gentle flexion exercises. Even 10 minutes a day can help.
- Don’t wait until you can’t walk at all. Early action means better outcomes.
Is neurogenic claudication the same as sciatica?
No. Sciatica is pain that radiates along the sciatic nerve, often from a herniated disc. It’s usually one-sided and sharp. Neurogenic claudication is caused by spinal canal narrowing and affects both legs in most cases. It’s not a sharp pain - it’s heaviness, cramping, or numbness that builds up during walking and improves with forward bending.
Can I still exercise with neurogenic claudication?
Yes - but you need to choose the right kind. Avoid exercises that arch your back, like back extensions or standing toe touches. Focus on flexion: walking with a walker, swimming on your back, seated forward bends, and stationary cycling. These open up the spinal canal and reduce pressure on the nerves. Many patients find they can walk farther over time with consistent, gentle movement.
Does an MRI always show spinal stenosis if I have neurogenic claudication?
No. Up to 67% of people over 60 show spinal narrowing on MRI even if they have no symptoms. That’s why diagnosis relies on matching your symptoms - like the shopping cart sign - with the imaging. A clear MRI doesn’t rule out stenosis, and a narrow canal on MRI doesn’t mean you need surgery. Your symptoms are the guide.
How long does it take to recover from spinal stenosis surgery?
Most people can walk without assistance within 4 to 6 weeks. Full recovery takes 3 to 6 months. You’ll need physical therapy to rebuild strength and learn safe movement patterns. Many patients report being able to walk longer distances and return to hobbies like gardening or walking their dog within 3 months after surgery.
Are there any warning signs that I need surgery sooner?
Yes. If you notice weakness in your legs, trouble lifting your feet (foot drop), loss of bladder or bowel control, or numbness in the groin area, these are red flags. These signs mean your nerves are under serious pressure. Don’t wait - see a spine specialist immediately. These are rare, but they require urgent evaluation.



8 Comments
Chrisna Bronkhorst
November 12, 2025 AT 01:40Stop calling it 'old age'-this is systemic medical negligence. They treat symptoms like trivia while the spine collapses like a bad IKEA shelf. You don't need more meds-you need a spine surgeon who reads beyond the MRI report.
Amie Wilde
November 13, 2025 AT 16:50I leaned on a cart for 2 years thinking it was just tired legs. Then my PT asked if I bent forward. I cried. It’s not aging. It’s treatable.
Gary Hattis
November 14, 2025 AT 10:55As someone who grew up in India and now lives in the US, I’ve seen both systems. In the US, they over-test and under-listen. In India, they under-test and over-prescribe. But this? This post nails it. The shopping cart sign isn’t folklore-it’s diagnostic gold. And yeah, cycling beats walking every time. My knees thank me.
Benjamin Stöffler
November 14, 2025 AT 16:10Let’s be precise: neurogenic claudication is not ‘nerve pain’-it’s radicular compression secondary to acquired spinal stenosis, typically degenerative, often exacerbated by lumbar lordosis and facet hypertrophy. The ‘shopping cart sign’ is merely a behavioral adaptation to decompress the neural foramina during flexion. You cannot diagnose this without dynamic imaging-static MRI is meaningless without correlation to positional symptoms. And no-gabapentin doesn’t fix anatomy. It just numbs the alarm system. The real issue? Most physiatrists haven’t touched a spinal canal since med school. Surgery isn’t a last resort-it’s the only anatomical correction when conservative care fails. Period.
Esperanza Decor
November 15, 2025 AT 02:15I started doing seated forward bends while watching TV. Just 5 minutes a night. After 3 weeks, I walked to the mailbox without stopping. I didn’t even know I could. Don’t wait for a doctor to validate your pain. Move your body the way it begs you to.
Deepa Lakshminarasimhan
November 15, 2025 AT 23:17They don’t want you to know this, but spinal stenosis is a government ploy to sell surgeries and drugs. MRI machines are expensive. They need to justify them. The ‘shopping cart sign’? That’s just people being smart. Real medicine is movement, fasting, and avoiding fluoride. They’ll never tell you that.
Erica Cruz
November 17, 2025 AT 22:43Wow. Another feel-good article for the over-50 crowd that ignores the real problem: lazy patients who won’t do real rehab and doctors who are too scared to say ‘you need to lose weight and stop sitting on your butt all day.’ This is just fear-mongering wrapped in medical jargon. My 72-year-old uncle walks 5 miles daily. He doesn’t need a cart. He needs a better lifestyle.
Johnson Abraham
November 19, 2025 AT 19:28bro i had this and the doc said ‘just walk more’ so i did… then i fell and broke my hip. now i got a metal butt. so yeah. maybe dont trust the cart thing. maybe just get the surgery. or dont. idk. 🤷♂️