Warfarin-TMP-SMX INR Risk Calculator
This tool estimates how much your INR might increase when taking Trimethoprim-Sulfamethoxazole (Bactrim/Septra) while on warfarin. Based on clinical studies, INR typically rises by 1.8 points on average.
Your Estimated INR After 48 Hours
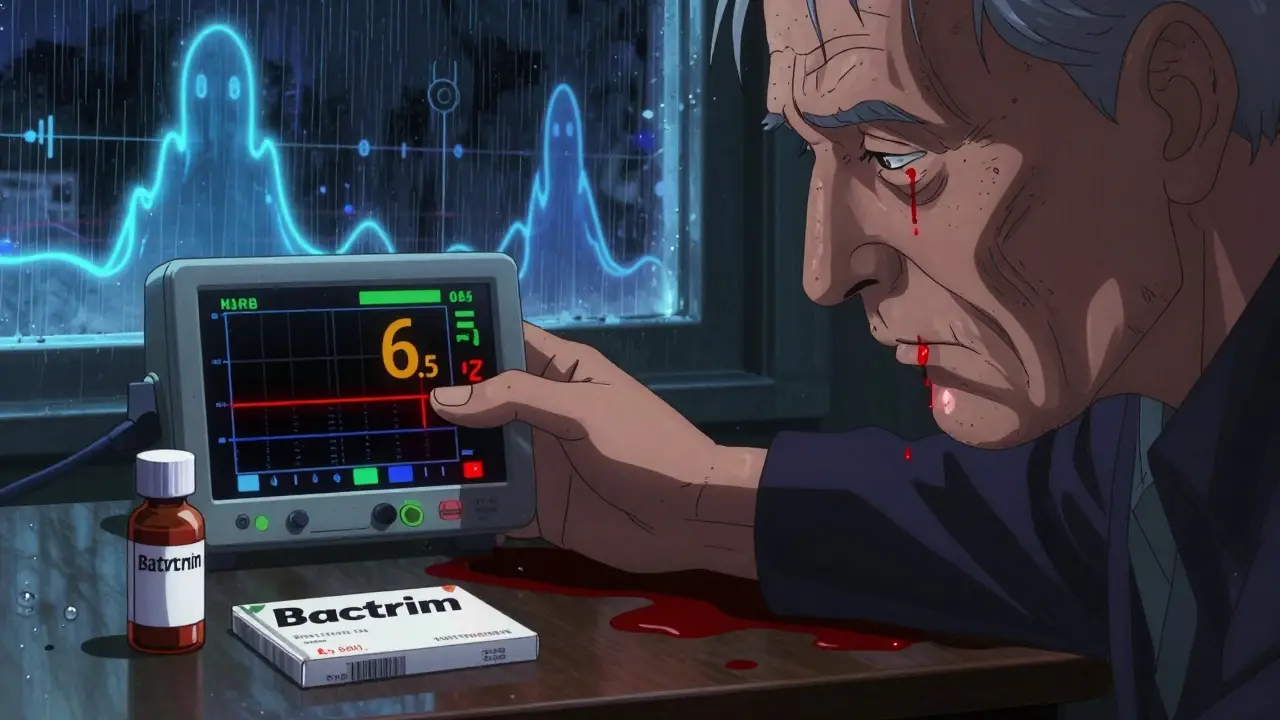
Imagine you're on warfarin to prevent strokes or manage a mechanical heart valve. Your INR is steady at 2.8 - you're in the safe zone. Then you get a urinary tract infection. Your doctor prescribes Trimethoprim-Sulfamethoxazole - also known as Bactrim or Septra. Three days later, you feel dizzy. You check your INR at home. It's 6.5. You're bleeding internally. This isn't rare. It happens more often than most people realize.
Why This Interaction Is So Dangerous
Warfarin is a blood thinner that works by blocking vitamin K, which your body needs to make clotting factors. It’s been around since the 1950s, and it’s still used by over 2.6 million Americans today. But warfarin doesn’t play nice with many other drugs. One of the worst offenders? Trimethoprim-Sulfamethoxazole (TMP-SMX).This antibiotic combination doesn’t just add to the effect of warfarin - it multiplies it. Studies show that when TMP-SMX is started, INR levels jump by an average of 1.8 points. That’s not a small blip. An INR above 4.0 means your blood takes much longer to clot. Above 5.0? Your risk of serious bleeding - like brain hemorrhage or gastrointestinal bleeding - shoots up sharply.
What’s happening inside your body? Three things at once:
- Trimethoprim blocks the CYP2C9 enzyme, which is responsible for breaking down the most powerful form of warfarin (S-warfarin). This means warfarin builds up in your blood.
- Sulfamethoxazole pushes warfarin off the proteins in your blood that normally hold it in place, making more of it free and active.
- Both parts of the drug can kill off good bacteria in your gut that make vitamin K - the very thing warfarin is trying to block.
This isn’t theoretical. A 2023 analysis of over 70,000 warfarin patients found that those taking TMP-SMX were far more likely to have dangerous INR spikes than those taking other antibiotics. Amoxicillin? INR rose by just 0.4 points. Ciprofloxacin? About 0.9. But TMP-SMX? Nearly double that.
Who’s Most at Risk?
Not everyone who takes TMP-SMX and warfarin will have a bad reaction. But some people are sitting on a ticking clock.Men are 9% more likely than women to experience INR spikes - no one knows exactly why, but it’s consistent across multiple studies.
Older adults? High risk. If you’re over 75, your liver doesn’t process drugs as well. Your body holds onto warfarin longer. Add TMP-SMX? INR can jump 2.5 points or more.
People with heart failure, liver disease, or poor nutrition are also vulnerable. If you’re not eating enough greens or getting enough vitamin K, your body has less buffer against warfarin’s effects. TMP-SMX removes what little buffer you have left.
And if you have a mechanical heart valve? You’re on warfarin for life. No room for error. One study found that 42% of patients who had INR spikes from TMP-SMX ended up in the hospital. Nearly 4% had fatal bleeding.
What the Experts Say
Dr. Gregory Makris, a leading hematologist, calls this interaction one of the most dangerous in clinical practice. He says: "TMP-SMX should be considered contraindicated in patients on warfarin unless absolutely necessary." That’s strong language. But the data backs it up. The Institute for Safe Medication Practices lists this combo as a high-alert interaction - meaning it can kill if not caught.Some doctors argue that if you monitor closely, you can use TMP-SMX safely. Dr. Jack Ansell, a respected hematologist, agrees - but only if you check INR within 48 hours of starting the antibiotic. No waiting. No hoping.
And here’s the kicker: even if you’ve taken TMP-SMX before without issues, that doesn’t mean it’s safe this time. Your body changes. Your liver slows down. Your diet shifts. Your INR baseline might be different. That’s why every single time matters.
What to Do If You Need an Antibiotic
If you’re on warfarin and get sick, don’t just take the first antibiotic your doctor suggests. Ask: "Is there a safer option?"For urinary tract infections, nitrofurantoin is a much safer choice. It doesn’t interfere with warfarin. For pneumonia or sinus infections, amoxicillin or doxycycline are often better options.
If TMP-SMX is your only option - maybe you’re allergic to everything else - here’s what your care team should do:
- Check your INR before starting the antibiotic.
- Reduce your warfarin dose by 20-30% preemptively, especially if you’re over 70 or have other risk factors.
- Test your INR again within 48-72 hours - not a week later.
- Test every 3-4 days while you’re on the antibiotic.
And if your INR climbs too high? Here’s the action plan:
- INR 4.0-5.0 with no bleeding: Skip 1-2 warfarin doses, then restart at a lower dose.
- INR 5.0-10.0 with minor bleeding (bruising, nosebleeds): Take 1-2.5 mg of oral vitamin K.
- INR over 10.0 or major bleeding (vomiting blood, black stools, sudden headache): Get IV vitamin K (5-10 mg) and 4-factor prothrombin complex concentrate - right away.
Don’t wait. Don’t call your doctor tomorrow. Go to the ER. This isn’t something you can manage at home.
Real Stories Behind the Numbers
A 78-year-old man with a mechanical aortic valve was prescribed TMP-SMX for a lung infection. His INR was 2.6. Three days later, it was 8.2. He ended up in the ICU with internal bleeding. He survived - but barely.A nurse practitioner in Florida told of three elderly women in her clinic who all had INR spikes from Bactrim. One had a brain bleed. Another lost 40% of her blood volume. Both needed transfusions.
And yet, a pharmacist on a medical forum said he’s seen patients take TMP-SMX for weeks with no change in INR. That’s true - some people don’t react. But you can’t assume you’re one of them. One bad reaction is enough.
Why This Still Matters in 2026
You might think: "Aren’t we all on those new blood thinners now?"Not even close. Over 1.2 million Americans with mechanical heart valves must stay on warfarin - the newer drugs don’t work for them. And while direct oral anticoagulants (DOACs) have replaced warfarin for many, about 2.6 million people still take it. That’s 1 in 13 adults on blood thinners.
And TMP-SMX? It’s still the 47th most prescribed antibiotic in the U.S. Doctors reach for it because it’s cheap, effective, and widely available. But they don’t always remember the risk.
A 2022 study found that nearly 1 in 5 warfarin patients got an interacting antibiotic within 30 days. And TMP-SMX made up almost 3 out of every 10 of those prescriptions.
The FDA updated warfarin’s label in 2019 to highlight this interaction. The American College of Chest Physicians says: "Avoid TMP-SMX if possible." Yet it still happens. Because no one checks. No one asks. No one warns.
What You Can Do Right Now
If you’re on warfarin:- Keep a list of all your meds - including antibiotics - and show it to every doctor.
- Ask: "Is this antibiotic safe with warfarin?" before you leave the office.
- If you’re prescribed TMP-SMX, insist on an INR check within 48 hours.
- Know the signs of bleeding: unusual bruising, pink or red urine, black stools, headaches, dizziness.
- Carry a medical alert card or wear a bracelet that says "On Warfarin - Avoid TMP-SMX."
And if you’re a caregiver for someone on warfarin? Don’t assume they know the risks. Explain it simply: "This antibiotic can make your blood too thin. We have to check your numbers early - or you could end up in the hospital." That conversation could save a life.
Can I take Bactrim if I’m on warfarin?
It’s not recommended. Bactrim (Trimethoprim-Sulfamethoxazole) can cause your INR to spike dangerously high, increasing your risk of serious bleeding. If you absolutely need an antibiotic and no safer option exists, your doctor should lower your warfarin dose before starting Bactrim and check your INR within 48 hours. Always ask for alternatives like nitrofurantoin or amoxicillin first.
How quickly does INR rise after starting TMP-SMX?
INR typically begins rising within 24-36 hours after starting TMP-SMX, with the peak effect usually seen between 48 and 72 hours. This is why checking your INR within 48 hours is critical - waiting longer could mean missing the window to prevent a dangerous spike.
What antibiotics are safe with warfarin?
Amoxicillin, doxycycline, and nitrofurantoin are generally considered safe with warfarin and cause little to no INR change. Azithromycin is also low-risk. Always confirm with your doctor or anticoagulation clinic - even "safe" antibiotics can vary in effect depending on your individual metabolism.
What should I do if my INR goes above 5.0?
If your INR is above 5.0 and you have no bleeding, take 1-2.5 mg of oral vitamin K and skip your next 1-2 warfarin doses. If you’re bleeding - even mildly, like nosebleeds or bruising - go to the ER immediately. For INR over 10 or major bleeding, you need IV vitamin K and 4-factor prothrombin complex concentrate. Don’t wait.
Do newer blood thinners avoid this interaction?
Yes - direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, and dabigatran don’t interact with TMP-SMX the way warfarin does. But if you have a mechanical heart valve, you can’t switch to a DOAC. You must stay on warfarin, which makes avoiding TMP-SMX even more critical.
Final Thought: Don’t Assume It’s Safe
This isn’t about being paranoid. It’s about being informed. Warfarin is a powerful drug. TMP-SMX is a common antibiotic. Together, they’re a silent threat. Thousands of people have been hospitalized - and some have died - because no one checked the INR in time.You can’t control every variable. But you can control this: ask the question. Get the test. Know the signs. If you’re on warfarin, your life depends on it.


9 Comments
Joy F
January 4, 2026 AT 01:02Let’s be real-this isn’t just a drug interaction, it’s a systemic failure. We’ve got a 70-year-old warfarin patient getting Bactrim like it’s Advil, and no one’s checking INR until they’re in the ER with a hemorrhagic stroke. The system doesn’t care until someone dies. And then? Another article like this pops up. We’re not fixing the problem-we’re just documenting the body count. This is medical malpractice dressed up as ‘standard care.’
Angela Fisher
January 6, 2026 AT 00:48EVERY SINGLE TIME. I KNEW IT. I TOLD MY DOCTOR. I SAID 'DON'T GIVE ME BACTRIM'-HE LAUGHED. THEN MY HUSBAND GOT IT FOR A UTI AND HIS INR WENT TO 9.3. THEY HAD TO GIVE HIM VITAMIN K IN THE ER. I SWEAR TO GOD, THE PHARMA COMPANIES KNOW THIS. THEY JUST DON'T CARE. THEY MAKE MORE MONEY WHEN YOU'RE IN THE HOSPITAL. THEY WANT YOU BLEEDING. I'M NOT CRAZY. I'M JUST A WIDOW.
Neela Sharma
January 7, 2026 AT 19:03Warfarin is a dance with death and TMP-SMX is the partner who pushes you off the cliff
But here’s the truth-we’re all just trying to survive
My aunt took this combo and lived
But she never ate greens again
And she checks her INR like it’s a prayer
Maybe safety isn’t about avoiding danger
But learning how to bow to it
Wren Hamley
January 9, 2026 AT 07:45Interesting breakdown, but I’m curious about the pharmacokinetic variability-why do some patients show zero INR elevation while others crash? Is it CYP2C9 polymorphism? Gut microbiome differences? Albumin binding capacity? The 2023 study mentions ‘individual susceptibility’ but doesn’t dive into biomarkers. If we could identify high-risk genotypes (CYP2C9*2/*3, VKORC1 variants), we could preemptively avoid TMP-SMX instead of reacting after the fact. Precision medicine isn’t a buzzword here-it’s a lifeline.
veronica guillen giles
January 9, 2026 AT 11:40So let me get this straight-you’re telling me that in 2026, a doctor can still prescribe an antibiotic that’s basically a death sentence for 1 in 3 warfarin patients… and we’re still acting like this is normal?
Meanwhile, the same doctors are telling patients to ‘eat more kale’ to ‘balance their INR.’
Yeah, thanks. I’ll just add ‘don’t die from antibiotics’ to my daily meditation list.
Angela Goree
January 10, 2026 AT 08:30THIS IS WHY AMERICA IS FALLING APART!!!
!!DOCTORS AREN'T EVEN TRYING!!
!!THEY JUST GIVE OUT DRUGS LIKE CANDY!!
WE NEED TO BAN BACTRIM FOR WARFARIN PATIENTS-FULL STOP!!
NO MORE ‘MAYBE’-NO MORE ‘IF YOU’RE CAREFUL’-THIS IS MURDER BY PRESCRIPTION!!
AND WHY IS THIS STILL ALLOWED IN 2026?!
WE HAVE AI TO RECOMMEND MOVIES BUT CAN’T STOP A KILLER DRUG COMBO?!
MY GRANDPA ALMOST DIED BECAUSE OF THIS!!
AMERICA, WAKE UP!!
Haley Parizo
January 10, 2026 AT 17:26What’s wild is how this interaction exposes the entire myth of ‘evidence-based medicine.’
It’s not that the data doesn’t exist-it’s that the system ignores it until someone dies.
We have randomized trials, meta-analyses, FDA warnings, and yet TMP-SMX is still prescribed like it’s harmless.
This isn’t negligence-it’s institutionalized apathy.
And the worst part? The people who pay the price aren’t the ones writing the guidelines.
They’re the elderly, the poor, the uninsured-the ones who don’t have time to fight for their own safety.
We call this healthcare. But it’s just damage control with a white coat.
Shruti Badhwar
January 11, 2026 AT 21:13As a nurse in Mumbai, I’ve seen this exact scenario play out with Indian patients on warfarin after valve replacements. Many don’t have access to regular INR monitoring. Antibiotics are often bought over the counter. Bactrim is cheap, available, and commonly used for fever and UTIs. No one tells them about the risk. I’ve had to call patients at 2 a.m. because their INR spiked. We need community education-not just clinical guidelines. Doctors can’t be everywhere. But awareness? That can be spread.
Liam Tanner
January 13, 2026 AT 04:30One of the most under-discussed truths: if you’re on warfarin and your doctor prescribes TMP-SMX, you’re not being cared for-you’re being convenience-tested. The real question isn’t whether the interaction exists. It’s why the system still allows it to happen. We need mandatory alerts in EHRs, pharmacist-led warfarin reviews before antibiotic scripts are filled, and patient handouts in 10 languages. This isn’t rocket science. It’s basic safety. And it’s still not happening.