Cumulative Drug Toxicity Calculator
Calculate your cumulative exposure to long-term medications. This tool estimates risk based on medical guidelines for drugs known to accumulate in the body.
Your Cumulative Exposure
Think about this: you’ve been taking the same pill every day for years. No big deal, right? But what if that pill, over time, is quietly building up in your body - not helping anymore, but hurting? That’s cumulative drug toxicity. It’s not a sudden reaction. It’s a slow leak. A silent storm. And it’s happening to millions of people on long-term medications.
What Exactly Is Cumulative Drug Toxicity?
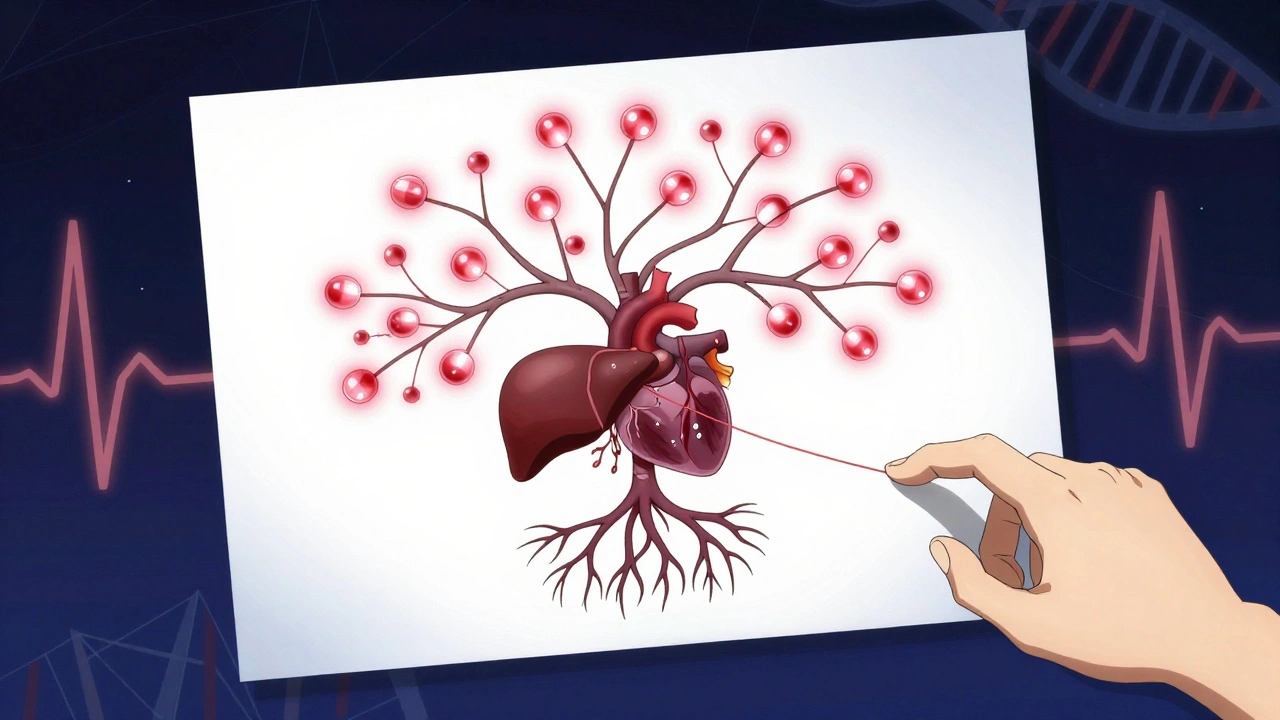
Cumulative drug toxicity happens when your body takes in more of a drug than it can get rid of. Over days, weeks, or even years, the drug builds up in your tissues - especially in fat and bone - until it crosses a line from therapeutic to toxic. It’s not about taking too much at once. It’s about taking the right dose, over and over, until your body can’t keep up.Drugs with long half-lives - meaning they stick around in your system for more than 24 hours - are the biggest culprits. Think amiodarone for heart rhythm, lithium for bipolar disorder, or digoxin for heart failure. These aren’t fast-clearing drugs. They linger. And if your liver or kidneys aren’t working perfectly - which is common as we age - they linger even longer.
Even vitamins can do this. Fat-soluble vitamins like A, D, E, and K don’t flush out easily. Take too much for too long, and they start damaging your organs. Same goes for heavy metals like lead or mercury - not from pills, but from environmental exposure - they accumulate in bone and brain tissue over decades.
Why It’s Hard to Spot
Unlike a drug allergy or overdose, where symptoms hit fast - nausea, rash, dizziness - cumulative toxicity creeps in. You might feel a little tired. Your hands might shake a bit more. Your memory isn’t as sharp. You blame it on stress, aging, or lack of sleep. But it’s the medication.Here’s the scary part: standard blood tests often miss it. A doctor checks your drug level and sees it’s "within range." But that’s just a snapshot. It doesn’t show how much has built up over the last six months or two years. That’s why patients on long-term amiodarone can develop lung scarring after hitting a cumulative dose of 600 grams - even if every monthly blood test looked fine.
A 2019 study from the Journal of the National Cancer Institute found that for cancer patients on targeted therapies, the chance of severe side effects jumped from 25% in the first treatment cycle to over 50% by the sixth. That’s not random. That’s accumulation. Each dose adds to the last. The body doesn’t reset.
Who’s at Highest Risk?
It’s not just older adults - though they’re the most affected. The American Geriatrics Society’s Beers Criteria lists 34 medications with high risk for cumulative toxicity in people over 65. But younger people aren’t safe either.- People with kidney or liver disease - their bodies clear drugs 30% to 50% slower.
- Those taking multiple medications - interactions can slow metabolism even more.
- Patients on chronic therapies: anticoagulants like warfarin, antibiotics like vancomycin, chemotherapy agents like doxorubicin.
- Anyone with genetic variations in liver enzymes - some people naturally process drugs slower.
And here’s something rarely talked about: lifestyle matters. Poor diet, alcohol use, and exposure to environmental toxins - pesticides, air pollution - can overload your detox systems. Ayurvedic medicine calls this "Dushi Visha" - chronic, low-grade poison from daily exposure. Modern science agrees: your body has limits.

Real Cases, Real Consequences
On Reddit’s r/medicine, an oncologist shared a case: a patient on amiodarone for 12 years developed severe lung fibrosis. Every test looked normal. The cumulative dose? Over 600 grams. That’s the tipping point. By the time symptoms showed up, the damage was irreversible.The FDA’s adverse event database recorded over 12,000 cumulative toxicity reports between 2018 and 2022. Nearly half involved blood thinners. A third involved heart meds. These aren’t rare. They’re predictable.
And it’s not just hospitals. A 2022 Medscape survey of 1,200 doctors found 67% had seen at least one serious case of cumulative toxicity in the past year. And 82% blamed patients for missing follow-up blood tests or skipping appointments. But why? Because no one told them the side effects might not show up until year three.
How Doctors Are Fighting Back
Some clinics are getting smarter. In rheumatology practices, tracking cumulative methotrexate doses cut adverse events by 37%. Oncology centers now use prediction tables to estimate toxicity risk after each cycle. The FDA now requires cumulative dose warnings on 78% of new cancer drugs - up from 52% just six years ago.Therapeutic drug monitoring (TDM) is becoming standard for high-risk meds. That means regular blood tests - not just to check if the level is "in range," but to track how much has built up over time. Digoxin, lithium, aminoglycosides - these drugs now come with clear cumulative dose limits.
For example: anthracycline chemotherapy (used for breast cancer and lymphoma) has a hard cap. Lifetime dose shouldn’t exceed 450 mg/m². Exceed that, and your heart’s at serious risk. That limit? Based on 17 studies with over 8,500 patients. It’s not guesswork. It’s science.
What You Can Do
If you’re on a medication long-term, here’s what to ask your doctor:- Is this drug known to build up in the body?
- Is there a cumulative dose limit I should know about?
- Do I need regular blood tests to check for buildup - not just for effectiveness, but for toxicity?
- Could my liver or kidneys be slowing how it clears?
- Are there alternatives that don’t accumulate?
Keep a personal log. Write down every pill you take, the dose, and when you started. Bring it to every appointment. Pharmacists can help calculate cumulative doses - especially for drugs like methotrexate or amiodarone. Many pharmacies now have systems to flag high cumulative exposures.
Don’t assume "no symptoms = no problem." Cumulative toxicity doesn’t announce itself. It sneaks in.
The Bigger Picture
The global market for therapeutic drug monitoring is expected to hit $4.7 billion by 2028. Why? Because we’re living longer. More people are on multiple meds for decades. More chronic diseases. More drugs. More risk.Regulators are catching up. The European Medicines Agency now requires cumulative toxicity assessments for all new drugs meant for long-term use - starting January 2024. AI models are being tested to predict individual risk by analyzing 27 different factors - metabolism speed, genetics, organ function, even diet.
But technology won’t fix this alone. We need better education. Patients need to understand: taking a pill every day isn’t harmless. It’s a long-term commitment - to your body’s ability to handle it.
The cost of ignoring this? Over $1.2 billion a year in the U.S. alone - from hospital stays, lost work, emergency visits. And that’s just cancer drugs. Add heart meds, psychiatric drugs, antibiotics… the number climbs.
Safe medication use isn’t just about getting the right dose. It’s about knowing how your body changes over time - and how drugs change with it.
When to Worry
You don’t need to panic. But if you’ve been on a medication for more than a year - especially if it’s for a chronic condition - and you’ve noticed new symptoms, ask these questions:- Did this start slowly, not suddenly?
- Is it something vague - fatigue, memory issues, tingling, unexplained weight loss?
- Is it getting worse, even though I haven’t changed my dose?
If yes, talk to your doctor. Bring your pill log. Ask about cumulative toxicity. Don’t wait until it’s too late.
Can cumulative drug toxicity be reversed?
Sometimes, yes - but not always. If caught early, stopping the drug and supporting organ function (like hydration, liver support) can help the body clear the buildup. But if damage has already occurred - like lung scarring from amiodarone or heart muscle damage from chemotherapy - it may be permanent. Early detection is key.
Do over-the-counter drugs cause cumulative toxicity?
Yes. Acetaminophen (Tylenol) is the most common example. Taking more than 3,000 mg a day for weeks can cause silent liver damage. Herbal supplements like kava or comfrey can also build up and harm the liver. Even high-dose vitamin D over months can lead to calcium deposits in blood vessels and kidneys. Just because it’s sold without a prescription doesn’t mean it’s safe long-term.
Why don’t doctors always check for cumulative toxicity?
Many don’t realize how common it is. Others assume standard blood tests are enough. Some systems don’t track cumulative doses automatically. And time is short in clinics. But awareness is growing. Pharmacists and specialized clinics are leading the charge - and patients who ask the right questions are getting better care.
Are some people genetically more at risk?
Absolutely. Genetic differences in liver enzymes - like CYP2D6 or CYP3A4 - affect how fast you break down drugs. Some people are slow metabolizers. They clear drugs slowly, so even normal doses build up. Genetic testing isn’t routine yet, but if you’ve had unexpected side effects from multiple medications, it’s worth discussing.
How long does it take for a drug to build up to toxic levels?
It varies. For drugs with short half-lives, maybe weeks. For fat-soluble drugs like amiodarone or lithium, it can take months or years. Amiodarone’s half-life is 50-100 days - meaning it takes 5-10 months to reach steady state. Toxicity often appears after 6-12 months of daily use. There’s no universal timeline - it depends on the drug, your body, and your health.
Medication isn’t a one-time fix. It’s a long-term partnership with your body. The more you understand how drugs behave over time, the better you can protect yourself. Don’t wait for a crisis. Ask the questions now - before the side effects become permanent.


15 Comments
Lynn Steiner
December 2, 2025 AT 11:46I've been on lithium for 8 years and my hands shake so bad I can't hold a coffee cup. They told me it's 'within range'... but range for who? The drug company? I'm crying in the kitchen every morning and they call it 'normal'.
Alicia Marks
December 2, 2025 AT 18:10You're not alone. I started tracking my meds in a little notebook after my mom had kidney damage from amiodarone. It saved my life. Just write it down. You got this.
Paul Keller
December 4, 2025 AT 05:16While I appreciate the anecdotal nature of this post, it is imperative to recognize that cumulative drug toxicity represents a significant paradigm shift in pharmacovigilance. The pharmacokinetic modeling of long-half-life compounds necessitates a longitudinal, patient-centric approach to therapeutic monitoring, which remains underutilized in primary care settings due to systemic inefficiencies and reimbursement constraints. This is not merely a clinical issue-it is a structural failure of healthcare delivery.
Jay Everett
December 5, 2025 AT 01:18Bro. This is wild. I used to think meds were like coffee-take it, feel better, done. But nah. It’s more like leaving a candle burning in your closet for 10 years. One day you smell smoke… and the whole damn house is on fire. 🕯️🔥 I’ve seen people on methotrexate for RA turn into ghosts by year 5. No one warned them. No one checks the numbers. Just ‘you’re fine’ while their liver screams. We need to stop treating bodies like machines that don’t rust.
Rebecca M.
December 6, 2025 AT 22:20Oh wow, so now we’re blaming the pills for everything? Maybe if people just ate less sugar and did yoga, they wouldn’t need 17 pills a day? 🙄 I bet this is why we’re all so tired-because we’re too lazy to ‘live healthy’.
dave nevogt
December 8, 2025 AT 04:59There’s something deeply human about this. We take pills not just to heal, but to outrun mortality. We swallow time. Every tablet is a small rebellion against decay. But the body remembers. It doesn’t forget. And when it finally breaks, it doesn’t scream-it just… slows down. A tremor. A pause. A forgotten word. We call it aging. But maybe it’s just accumulation. Maybe we’re all just slowly poisoning ourselves with good intentions.
Arun kumar
December 9, 2025 AT 08:54in india we call this 'jharay ki bimari' - disease from slow poison. grandmas knew this. they said dont take too many pills for long time. now doctors say 'its fine' but body says no. i lost my uncle to liver failure from painkillers he took for back pain for 7 years. no one warned him.
Zed theMartian
December 10, 2025 AT 19:30Ah yes, the classic ‘pharma conspiracy’ narrative. Let me guess-next you’ll tell us fluoride in water causes dementia and 5G fries your mitochondria? This is just fearmongering dressed up as medical insight. If your body can’t handle a therapeutic dose after a year, maybe you shouldn’t be on it. Blame the patient, not the science.
Ella van Rij
December 10, 2025 AT 21:15I mean… it’s cute that you think doctors are *supposed* to track cumulative doses. Like they have time between their 14 Zoom calls and their 3rd glass of wine. I once asked my rheumatologist about my methotrexate total and she said, ‘Honey, I just refill the script.’ 🙃
ATUL BHARDWAJ
December 12, 2025 AT 00:01In India, elders say: medicine is like salt. A little helps. Too much kills. No need for charts. Just listen to your body.
Steve World Shopping
December 13, 2025 AT 13:20This is a classic case of bioaccumulation pathology driven by polypharmacy-induced metabolic overload. The hepatic CYP450 system is being chronically saturated, resulting in nonlinear pharmacokinetics and off-target organ deposition. You're essentially creating a pharmacological time bomb by ignoring clearance kinetics. This is not anecdotal-it's biostatistical inevitability.
Elizabeth Grace
December 14, 2025 AT 14:37I took vitamin D for 2 years because my doctor said I was deficient. Turns out I had calcium deposits in my arteries. Now I can't even walk without pain. I thought it was ‘good’ because it was a vitamin. How is that not a crime?
Steve Enck
December 15, 2025 AT 23:12The structural violence of modern pharmacotherapy cannot be overstated. The neoliberal medical-industrial complex commodifies patient vulnerability, transforming chronic illness into a revenue stream. Cumulative toxicity is not an accident-it is the predictable outcome of a system that prioritizes adherence metrics over physiological integrity. We are not patients. We are data points with pill schedules.
मनोज कुमार
December 16, 2025 AT 19:32Doctors dont care its all about sales and profit no one checks cummulative dose just give more pills
Joel Deang
December 17, 2025 AT 08:34my grandma took digoxin for 15 years. she forgot her own name but said ‘i feel fine’ every time the dr came. she died with a heart rate of 42. they said it was ‘natural aging’. i know better now. i keep a log. you should too. ❤️