Switching from a brand-name drug to a generic version seems like a simple way to save money. For most medications, it works fine. But when it comes to NTI drugs, that switch can be risky-sometimes dangerously so. NTI stands for narrow therapeutic index. These are drugs where the difference between a helpful dose and a toxic one is razor-thin. A tiny change in how much of the drug enters your bloodstream can mean the difference between healing and hospitalization.
What Makes a Drug an NTI Drug?
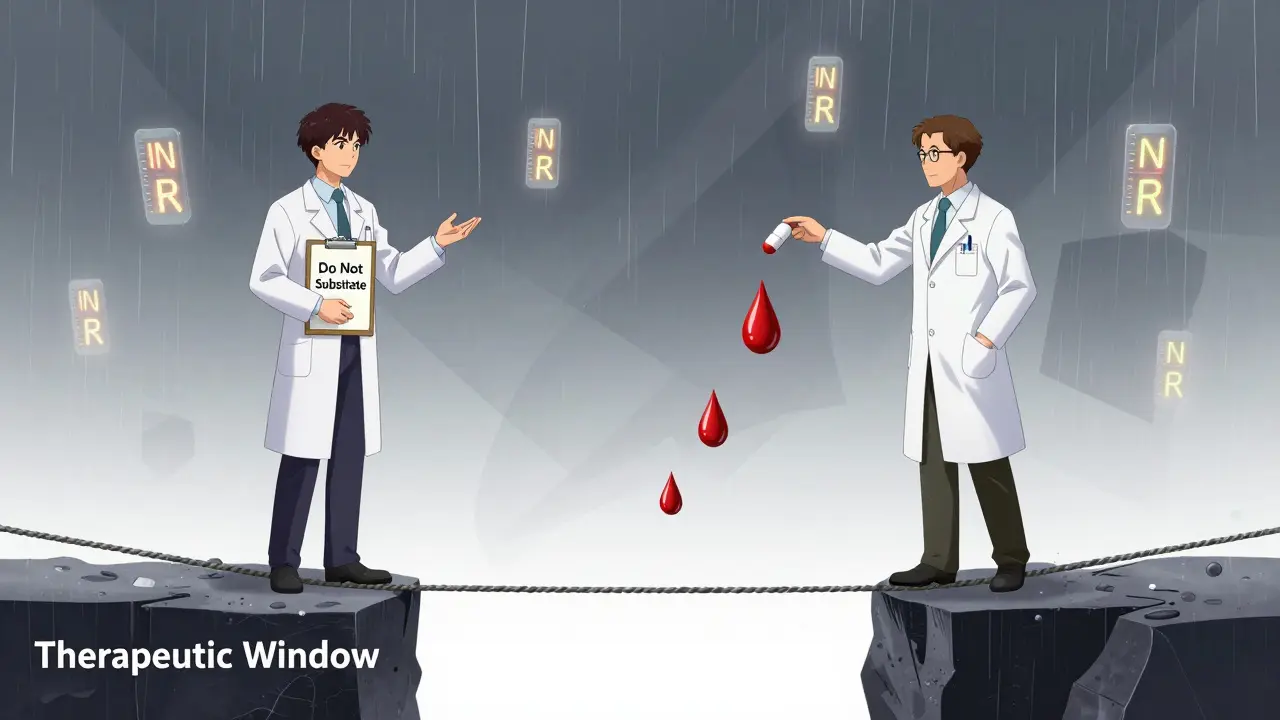
An NTI drug has a therapeutic window so small that even a 10% shift in blood concentration can cause harm. The FDA defines these as drugs where small changes in dose or blood levels can lead to serious treatment failures or dangerous side effects. Think of it like walking a tightrope. One misstep, and you fall.
Examples include warfarin (a blood thinner), phenytoin (for seizures), lithium (for bipolar disorder), digoxin (for heart failure), and methadone (for pain or opioid addiction). For warfarin, the target INR range is 2.0 to 3.0. Go below 2.0, and you risk a clot. Go above 3.0, and you risk bleeding. That’s a narrow margin. Phenytoin’s safe range is 10 to 20 mcg/mL. Above 20, you get dizziness, tremors, even coma.
These drugs aren’t rare. Roughly 15 to 20% of commonly prescribed medications fall into this category. And many of them are now available as generics-cheaper, yes, but not always identical in how your body handles them.
The Bioequivalence Problem
When the FDA approves a generic drug, it must prove it’s “bioequivalent” to the brand version. That means the generic must deliver between 80% and 125% of the active ingredient into your bloodstream compared to the original. Sounds fair? Not for NTI drugs.
Let’s say your brand-name warfarin delivers exactly 5 mg of the drug into your blood. A generic version could deliver as little as 4 mg or as much as 6.25 mg-and still pass FDA approval. That’s a 56% swing in actual dose. For a drug where 0.5 mg too much can cause bleeding, that’s not a small difference. It’s a life-or-death gap.
The FDA admits this. In fact, they’ve said for NTI drugs, “tighter bioequivalence limits” should be used. But they haven’t changed the rules yet. So right now, a generic warfarin tablet that’s 125% as potent as the brand is still considered “equivalent.” That’s not equivalence. It’s a gamble.
Real Cases, Real Consequences
This isn’t theoretical. There are documented cases of patients having seizures after switching from brand-name carbamazepine to a generic version. Others experienced toxic levels of phenytoin after a pharmacy switch-nystagmus, confusion, loss of coordination. In one study, patients on warfarin saw their INR drop sharply after switching from Coumadin to a generic, increasing clot risk. In another, INR spiked, leading to internal bleeding.
And it’s not just about the drug itself. Generic versions can vary in fillers, coatings, and manufacturing processes. These don’t affect the active ingredient-but they can change how quickly or completely the drug is absorbed. For someone on methadone, a slightly faster absorption could mean respiratory depression. For someone on lithium, a slight delay could mean a relapse into depression or mania.
Some studies say switching is fine. A 2007 study found no major issues with generic warfarin in a managed care setting. But those studies often ignore individual variability. What works for one person doesn’t work for another. One patient’s stable INR can become unstable after a single switch. And by then, the damage might already be done.
Who Decides? The Doctor, Not the Pharmacist
Pharmacists are trained to substitute generics when allowed by law. In many states, they can switch your medication without asking you or your doctor-unless the drug is on a restricted list. But for NTI drugs, that’s a problem.
The American Medical Association (AMA) has been clear: the prescribing physician should make the decision about whether to substitute an NTI drug. Why? Because they know your history, your labs, your risks. A pharmacist may not know you’ve had two recent clots or that your kidney function is declining.
Some states, like North Carolina, have laws that restrict automatic substitution for NTI drugs. But not all do. And even where restrictions exist, enforcement is inconsistent. Many patients never know they’ve been switched until they start feeling off.

What Patients Need to Know
If you take an NTI drug, here’s what you need to do:
- Know your drug. Is it on the list? Warfarin, phenytoin, lithium, digoxin, theophylline, methadone, levothyroxine-these are common ones.
- Ask your doctor: “Is this an NTI drug? Should I stay on the brand?”
- Check your prescription label. If it says “dispense as written” or “do not substitute,” that’s your protection.
- Never let a pharmacy switch your NTI drug without telling you. Ask them to confirm the name and manufacturer every time you fill it.
- Keep a written list of all your meds, including doses and manufacturers. Bring it to every appointment.
- For warfarin, get your INR checked more often after any switch-even if you feel fine.
Don’t assume generics are interchangeable. For NTI drugs, they’re not. A small change in absorption can have a big impact on your health.
The Bigger Picture
Generic drugs save billions in healthcare costs. That’s good. But not at the cost of patient safety. The current system treats all drugs the same. That’s outdated. We need a smarter approach: stricter bioequivalence standards for NTI drugs, mandatory physician consent for substitution, and better tracking of patient outcomes after switches.
Some experts argue that generic substitution should be banned for NTI drugs entirely. Others say better monitoring can make it safe. The truth? We don’t have enough real-world data. The American Society for Clinical Pharmacology and Therapeutics has called for more research-empirical evidence of risk, not just theory.
Until then, the safest path is simple: if you’re on an NTI drug, don’t let anyone switch it without your doctor’s approval. Your life may depend on it.
What does NTI mean in medication?
NTI stands for Narrow Therapeutic Index. It means the difference between a safe, effective dose and a toxic dose is very small-usually a ratio of 2:1 or less. Even small changes in how much of the drug gets into your blood can cause serious side effects or treatment failure.
Which drugs are considered NTI drugs?
Common NTI drugs include warfarin (blood thinner), phenytoin (seizure control), lithium (bipolar disorder), digoxin (heart condition), theophylline (asthma), methadone (pain or addiction), and levothyroxine (thyroid replacement). These require careful dosing and regular monitoring.
Can I safely switch from brand-name to generic for an NTI drug?
It’s not recommended without your doctor’s approval. Even FDA-approved generics can vary in how your body absorbs them. For NTI drugs, those small differences can lead to serious health risks. Always ask your doctor before allowing a switch.
Why is the 80-125% bioequivalence range a problem for NTI drugs?
For most drugs, a 20% variation in blood levels is harmless. But for NTI drugs, that 20% can mean the difference between a therapeutic dose and a toxic one. A drug with a 2:1 therapeutic window can’t safely tolerate a 45% swing in absorption-yet that’s allowed under current FDA rules.
What should I do if my pharmacy switches my NTI drug without telling me?
Contact your doctor immediately. Ask for your medication to be switched back to the original brand or manufacturer. Request a blood test (like INR for warfarin or serum level for phenytoin) to check if your levels are still in range. Always ask for "dispense as written" on your prescription to prevent future switches.



13 Comments
Christine Joy Chicano
January 6, 2026 AT 18:41So let me get this straight-FDA lets a blood thinner vary by over 50% in potency and calls it ‘bioequivalent’? That’s not science, that’s Russian roulette with a prescription pad. I’ve seen patients on warfarin go from stable INRs to ER trips after a pharmacy switch. No one talks about this enough. The system is broken, and we’re the ones paying the price in bleeding ulcers and clots.
Adam Gainski
January 7, 2026 AT 00:57I work in a hospital pharmacy, and I’ve seen this firsthand. We’re supposed to substitute unless it’s marked ‘DAW 1’-but with NTI drugs, I always double-check with the prescriber. One nurse told me a patient on lithium started hallucinating after a generic switch. Turned out the new batch had a different dissolution rate. We’re not talking about aspirin here. This needs a policy overhaul.
Rachel Steward
January 8, 2026 AT 11:25Oh please. You’re all acting like generics are some sinister corporate plot. The FDA has reviewed thousands of studies. If generic phenytoin were that dangerous, we’d have a national crisis. You’re cherry-picking anecdotes and ignoring population-level data. Most patients switch without issue. The real problem? Overmedicated, under-monitored patients who don’t even know their own INR numbers. Blame the patient education gap, not the FDA.
Also, ‘dispense as written’? That’s a privilege for the wealthy. Most people can’t afford brand-name warfarin. Your fearmongering is classist disguised as medical concern.
Alex Danner
January 9, 2026 AT 19:46Let me tell you about Mr. Henderson. 78. On digoxin for 12 years. Stable as a rock. Then one day, his pharmacy switched him to a generic. He started vomiting, dizzy, confused. Thought he was having a stroke. Got rushed in. His digoxin level was 3.8 ng/mL-TOXIC. Brand was 0.9. He didn’t even know he’d been switched. Took three weeks to stabilize. He’s still scared to leave the house. This isn’t theory. This is Tuesday in every ER across America.
Elen Pihlap
January 11, 2026 AT 11:27why do they even make generics if they’re not the same?? i just want to feel okay
Sai Ganesh
January 12, 2026 AT 00:10In India, we have the same issue with antiepileptics. Many patients on phenytoin switch to generics due to cost, and then we see breakthrough seizures. Doctors here often write ‘not interchangeable’ on scripts, but pharmacists still substitute. It’s a systemic failure-lack of awareness, lack of regulation, lack of follow-up. We need better labeling and mandatory patient counseling, not just laws.
Paul Mason
January 13, 2026 AT 09:43Oh for crying out loud, it’s just a pill. People used to take the same medicine for decades without knowing what brand it was. Now everyone’s a hypochondriac. If you’re on lithium and you’re worried, get your blood levels checked once a month. It’s not rocket science. Stop blaming the system. Take responsibility for your own health.
Katrina Morris
January 14, 2026 AT 15:34i just found out my levothyroxine was switched and i felt so off for weeks but thought it was stress or my period or something
now i always check the label and ask the pharmacist and i feel like a paranoid person but honestly better safe than sorry
Andrew N
January 15, 2026 AT 22:58Studies show no difference. End of story. You’re overreacting because you don’t understand pharmacokinetics. The 80-125% range is statistically sound. If your INR fluctuates after a switch, it’s probably because you missed a dose or ate kale. Stop blaming generics.
Jessie Ann Lambrecht
January 16, 2026 AT 06:00I’m a nurse practitioner and I’ve fought pharmacies over this too many times. I had a patient on methadone for chronic pain who started nodding off after a switch. We caught it because she came in with pinpoint pupils. The generic had a different coating-faster absorption. We had to re-taper her. I don’t care how much it costs. If it’s an NTI drug, I write ‘do not substitute’ in bold, red letters. Because I’ve seen what happens when we don’t.
Vince Nairn
January 17, 2026 AT 11:06So what you’re saying is… the government lets drug companies sell potentially lethal variations of life-saving meds because they’re cheaper? And we’re supposed to be grateful? Cool. Cool cool cool. I’m sure the CEOs are sleeping like babies. Meanwhile, grandma’s on warfarin and the pharmacy just swapped her pill like it was a candy bar. Welcome to America, folks. 🤡
Ayodeji Williams
January 18, 2026 AT 22:53bro generics are just as good 😎
u just scared of change
my cousin took generic lithium for 5 yrs no prob
u just wanna pay more for nothing 💸
Kyle King
January 19, 2026 AT 00:59They’re hiding the truth. The FDA is in bed with Big Pharma. Brand-name companies pay them to keep the rules loose so they can sell their own generics later under a different name. That’s why they won’t tighten the limits. This isn’t about safety-it’s about control. I’ve seen the leaked emails. The real NTI drugs? The ones they don’t tell you about.