Every year, Americans fill over 3.9 billion generic prescriptions. That’s 9 out of every 10 prescriptions written. And yet, most people still believe brand-name drugs are better. The truth? You’re paying way more for the same medicine - sometimes 85% more.
They’re the same drug. Really.
Generic drugs aren’t ‘weaker’ versions. They don’t have different ingredients. They don’t work slower. They’re not made in shoddy factories. A generic drug contains the exact same active ingredient, in the exact same strength, as the brand-name version. It’s the same chemical. Same dosage. Same way it’s taken - pill, injection, patch, you name it.
The FDA requires every generic to prove it works the same way in your body. That means it must deliver the same amount of medicine into your bloodstream at the same speed as the brand. The allowed difference? Just 80% to 125% of the brand’s performance. In real terms? That’s not a gap. That’s noise. It’s like comparing two identical cars with one having a slightly different shade of paint.
Manufacturers don’t get to skip testing because they’re lazy. They skip it because they don’t need to. The original brand already proved safety and effectiveness. Generics just prove they match it. No extra clinical trials. No retesting on humans. That’s why they cost less.
How much cheaper are generics?
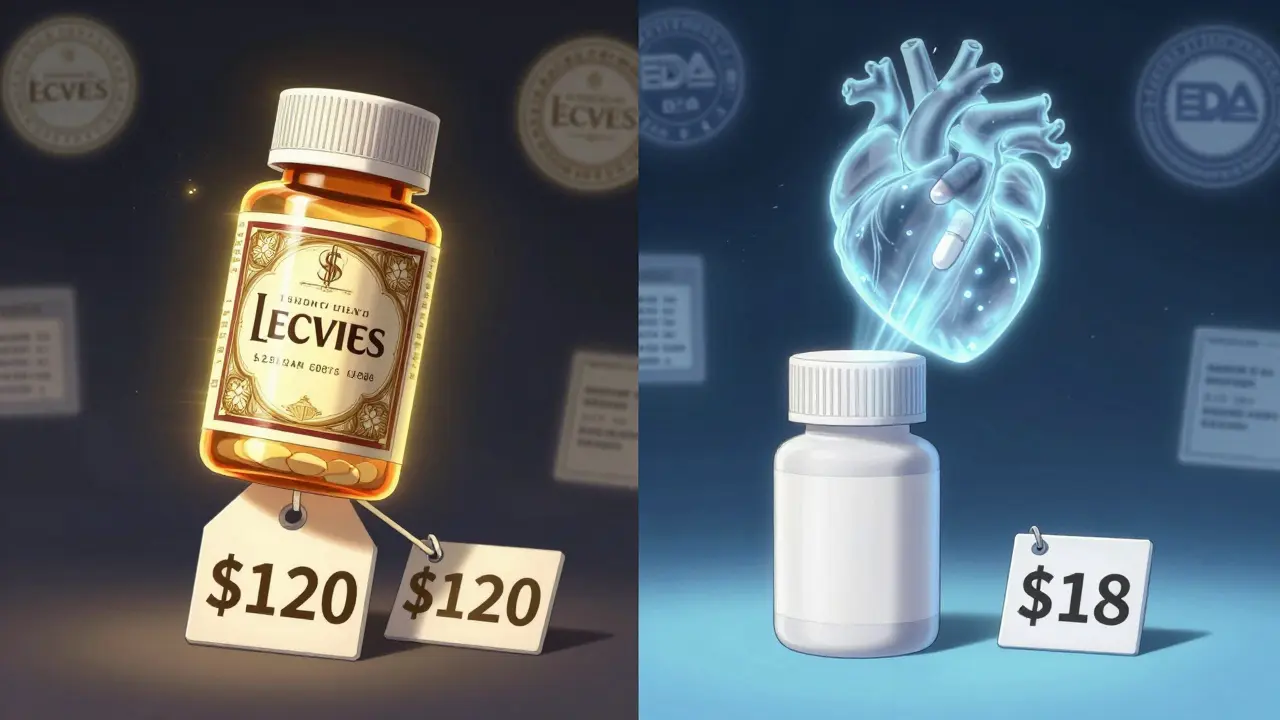
On average, generic drugs cost 79% to 85% less than their brand-name counterparts. That’s not a guess. That’s the FDA’s official estimate, backed by data from Tebra’s 2025 survey of over 1,000 Americans. One person told me they used to pay $120 a month for their brand-name blood pressure pill. Switched to generic? $18. That’s not a savings. That’s a life change.
And it gets better. The more generic versions enter the market, the cheaper it gets. With just one generic competitor, prices drop to about 90% of the original brand’s price. With three or four generics? Down to 60-70%. When five or more companies make the same drug? Prices often fall below half of what the brand charged.
Take Nexavar, a cancer drug. When the first generic hit in 2022, Bayer cut its own list price by 50% - not because they became charitable, but because they knew they couldn’t compete on price anymore. Merck did the same with Januvia, dropping prices by 42.4% before the new Medicare price caps even kicked in. These aren’t isolated cases. This is the pattern now.
Why do brand-name drugs cost so much?
Brand-name companies spend billions developing new drugs. That’s true. But here’s what nobody tells you: most of that cost isn’t recouped from the people who actually use the drug. It’s recouped from insurance companies, government programs, and middlemen who negotiate rebates.
That’s why you see crazy list prices - $1,000 a pill - but your copay is $20. The difference? That’s the rebate. Manufacturers give discounts to pharmacies, insurers, and pharmacy benefit managers (PBMs) to get their drug on the formulary. The list price is basically a starting point for negotiation. The real price - what’s actually paid - is called the net price.
In 2024, brand-name drug list prices went up 2.3%, but net prices only rose 0.1%. That means manufacturers are giving away more discounts just to stay in the game. Why? Because generics are everywhere. And they’re cheap. If you’re a brand and you don’t lower your price, you lose market share fast.

Why do people still choose brand names?
Eighty-four percent of Americans believe generics are just as effective. That’s good. But 62% still trust brand names more. Why? Because they’ve been told for decades that ‘name brands are better.’ It’s marketing. It’s habit. It’s fear.
One woman told me she switched to her generic thyroid med and felt ‘off’ for a week. She went back to the brand. Turns out, she’d been taking it on an empty stomach. The generic had a slightly different filler, and it affected absorption. She didn’t know. Her doctor didn’t know. It wasn’t the generic. It was how she took it.
Another guy refused his generic antidepressant because the pill looked different. ‘It’s not the same,’ he said. But the active ingredient? Identical. The color? Just dye. The shape? Just the mold. The effect? The same.
Most of the time, switching to generic works perfectly. But when it doesn’t? It’s rarely because the drug is different. It’s because of how it’s taken, or because someone’s body reacts to a tiny change in inactive ingredients - like fillers or coatings. That’s rare. But it happens. That’s why your doctor should know if you switch.
What’s changing in 2025 and beyond?
The Inflation Reduction Act is shaking things up. Starting January 2026, Medicare will cap the price of 10 high-cost brand drugs at 80% off their list price. That means manufacturers will have to cut prices again - or lose sales. Some are already doing it. Merck’s Januvia price drop in 2025? Analysts say it was a preview of what’s coming.
Also, Medicare Part D is changing. In 2025, your out-of-pocket costs for drugs will be capped at $2,000 a year. That’s huge. But here’s the catch: that cap applies to the amount you pay - not the drug’s list price. So if your brand-name drug costs $1,000 a month, and your copay is $200, you’re still hitting that cap faster than if you were on a $10 generic.
And it’s not just Medicare. States are pushing for more transparency. Some are banning ‘pay-for-delay’ deals - where brand companies pay generics to wait before launching. That’s happening less now, but it used to be common. Now, generics hit the market faster. Prices drop faster.
When should you stick with brand?
Almost never.
There are a few exceptions. Some drugs have a very narrow therapeutic window - meaning even tiny differences in how they’re absorbed can cause problems. Think blood thinners like warfarin, or seizure meds like phenytoin. In those cases, your doctor might recommend sticking with one version - brand or generic - and not switching back and forth.
But even then, it’s not because generics are worse. It’s because consistency matters. If you’ve been on the same brand for years and your levels are stable? Fine. Don’t switch unless you need to. But if you’re starting a new medication? Always ask for the generic. It’s safe. It’s effective. It’s cheaper.
And if you’re paying cash? Always compare prices. Sometimes the brand is cheaper at a different pharmacy. Use GoodRx or similar tools. But don’t assume the brand is better just because it’s more expensive.
What’s the big picture?
Generic drugs are the reason U.S. prescription spending is 18% lower than in Canada, Germany, the UK, France, and Japan - even though we pay more for brand-name drugs. How? Because 90% of prescriptions are generics. And they cost pennies.
Since 2019, the U.S. has spent $6.4 billion less on generic drugs - even though more people are using them. That’s billions saved. Billions that went to groceries, rent, gas, or savings instead of pill bottles.
Generics aren’t a compromise. They’re the smart choice. They’re the backbone of affordable healthcare. And they’re not going anywhere.
If you’re on a brand-name drug and you’re not sure why - ask your pharmacist. Ask your doctor. Ask yourself: ‘Am I paying more because it’s better - or because I’ve never been told otherwise?’
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generic drugs to meet the same strict standards for quality, purity, strength, and stability as brand-name drugs. They’re made in the same type of facilities, under the same rules. The only difference is the price.
Why do generic pills look different?
By law, generics can’t look exactly like the brand-name version - that would be trademark infringement. So they use different colors, shapes, or markings. But the active ingredient? Identical. The difference is only cosmetic.
Can I switch from brand to generic safely?
For most medications, yes. Millions of people switch every year without issue. But if you’re on a drug with a narrow therapeutic window - like warfarin, thyroid meds, or seizure drugs - talk to your doctor first. They may recommend sticking with one version to avoid any small changes in how your body responds.
Why is my generic drug sometimes more expensive than the brand?
It’s rare, but it happens. Sometimes, insurance plans have better deals on the brand name. Or the generic is in short supply. Or you’re at a pharmacy that charges more. Always check prices with GoodRx or your pharmacy’s price list. You might be surprised.
Do generics take longer to work?
No. Generics must prove they work in the body at the same speed and to the same extent as the brand. If they didn’t, the FDA wouldn’t approve them. Any delay you feel is likely psychological - or due to how you take the pill (with food, on an empty stomach, etc.).
Will my insurance cover generics?
Almost always - and at a lower cost. Most insurance plans have lower copays for generics. Some even require you to try the generic first before covering the brand. It’s standard practice.
Are all generics made in the same place?
No. Generics are made in factories all over the world - including the U.S., India, and China. But every factory, no matter where, must meet FDA standards. The FDA inspects these facilities regularly. If they don’t pass, the drugs can’t be sold in the U.S.
Can I ask my doctor to prescribe a generic?
Absolutely. In fact, you should. Always ask: ‘Is there a generic version?’ Most doctors will say yes - and will write the prescription for the generic unless there’s a medical reason not to.


14 Comments
Sean Feng
January 12, 2026 AT 05:04Generics are fine I guess. I mean if you’re not rich it’s probably your only option anyway.
Adewumi Gbotemi
January 12, 2026 AT 12:59Here in Nigeria, we don’t even have brand drugs most times. Only generics. And people live. No drama. Just medicine.
Jason Shriner
January 14, 2026 AT 06:39So let me get this straight - we pay $120 for a pill because some CEO needs a new yacht, but the actual chemical? Identical to the $18 version? Wow. Capitalism is a beautiful thing. 😐
Vincent Clarizio
January 15, 2026 AT 20:31Let’s be real - the entire pharmaceutical industry is built on psychological manipulation. They spend more on marketing than R&D. The brand-name drug isn’t better - it’s just better at making you believe it is. The FDA doesn’t care about your feelings, only bioequivalence. And yet we’ve been conditioned to equate price with quality. That’s not medicine, that’s behavioral economics on steroids. You think your $120 pill works better because the bottle has a fancy logo? That’s not science - that’s Pavlovian conditioning with a co-pay.
Alex Smith
January 16, 2026 AT 17:05Interesting how the same people who’ll argue over which smartphone is ‘better’ won’t even question why their blood pressure med costs 8x more than the identical one. You’d never buy a $1000 toaster that does the same thing as a $150 one. But pills? Somehow that’s different. The real scam isn’t the generic - it’s the myth.
Madhav Malhotra
January 18, 2026 AT 00:28In India, generics are the norm. We call them ‘copy drugs’ - but everyone knows they work. My uncle takes the same generic for diabetes as the brand, and he’s been fine for 10 years. No issues. Just saved a lot of money.
Priya Patel
January 19, 2026 AT 22:21I switched my antidepressant to generic and felt weird at first - turned out I was taking it with coffee. My brain was just confused. Once I fixed that, boom - same effect. Why do we assume the pill changed when it was us all along?
Christian Basel
January 20, 2026 AT 00:33The FDA’s 80–125% bioequivalence window is a regulatory loophole disguised as science. That’s a 45% variance - that’s not noise, that’s a fucking canyon. And you want me to believe that’s clinically insignificant? Please. You’re not a pharmacist, you’re a marketing drone.
Roshan Joy
January 21, 2026 AT 04:28My cousin in Delhi took a generic for TB - saved her family from bankruptcy. The drug worked. The pill looked different. That’s it. 🙏
Michael Patterson
January 21, 2026 AT 06:24generics are dangerous bro. i had a friend who took a generic for epilepsy and he had a seizure. it was the pill. not him. the pill. the fda is lying. they dont test enough. trust me i read it on a forum.
Matthew Miller
January 22, 2026 AT 20:20You’re all naive. The FDA is a puppet of Big Pharma. The ‘bioequivalence’ standards are rigged. The real reason generics are cheaper is because they’re made in sweatshops with unregulated ingredients. You think your $18 pill isn’t full of talc and sawdust? Wake up. This isn’t healthcare - it’s a Ponzi scheme.
Alfred Schmidt
January 23, 2026 AT 19:36I switched to generic levothyroxine… and I cried for three days. I felt like my soul was being drained. I went back to the brand. I’m not crazy - the generic is evil. The fillers are cursed. I know it. I feel it. My thyroid knows. Why won’t anyone listen?!
Priscilla Kraft
January 24, 2026 AT 10:13For most people, generics are perfect. But if you’re on something like warfarin or thyroid meds, consistency matters. Stick with one version - brand or generic - and don’t switch back and forth. Talk to your pharmacist. They’ll help you pick the right one. 💡
Sam Davies
January 25, 2026 AT 04:20How quaint. Americans still believe in the myth of ‘brand superiority’. In Europe, we just take the cheapest thing that works - and we don’t need a 3,000-word essay to justify it. The real tragedy? You’re not paying more because you’re informed. You’re paying more because you’re lazy.