By the time you turn 70, there’s a better than even chance you’re struggling to hear conversations in a crowded room - not because people are mumbling, but because your ears have changed. This isn’t just normal aging; it’s presbycusis, the medical term for age-related hearing loss. It’s not something you can reverse, but it’s absolutely something you can manage - and doing so early can change your life.
What Presbycusis Really Feels Like
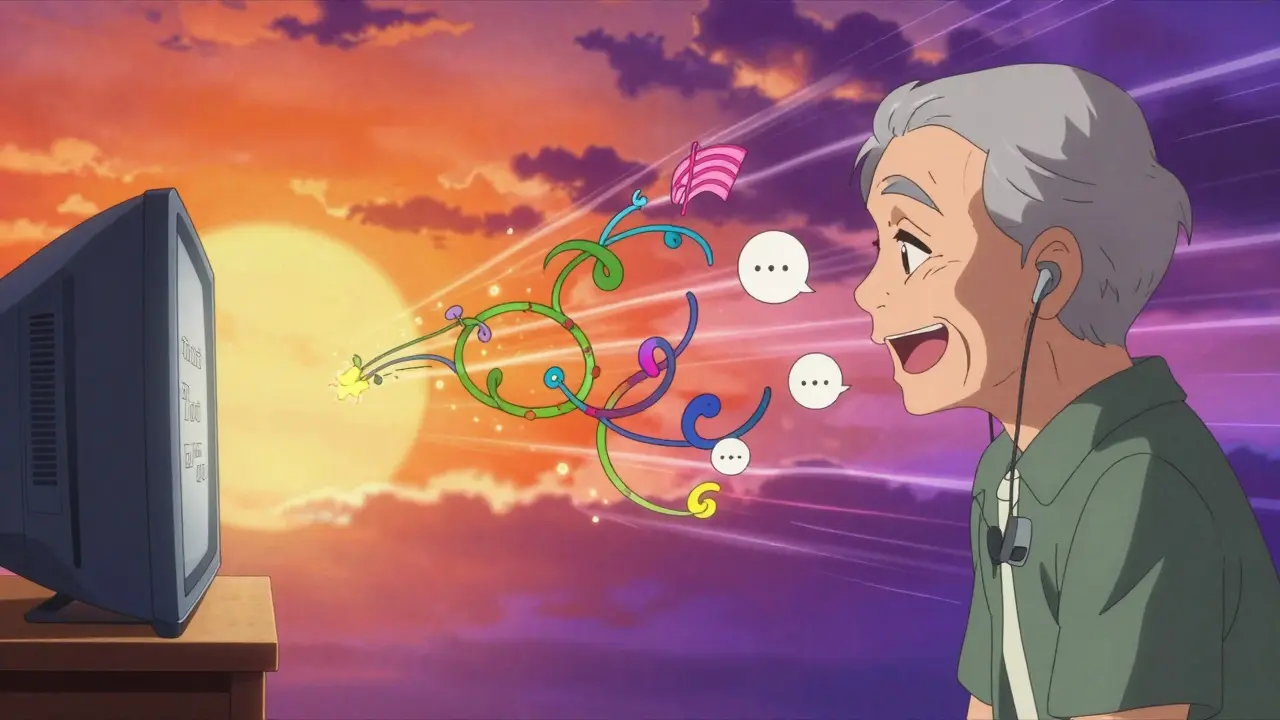
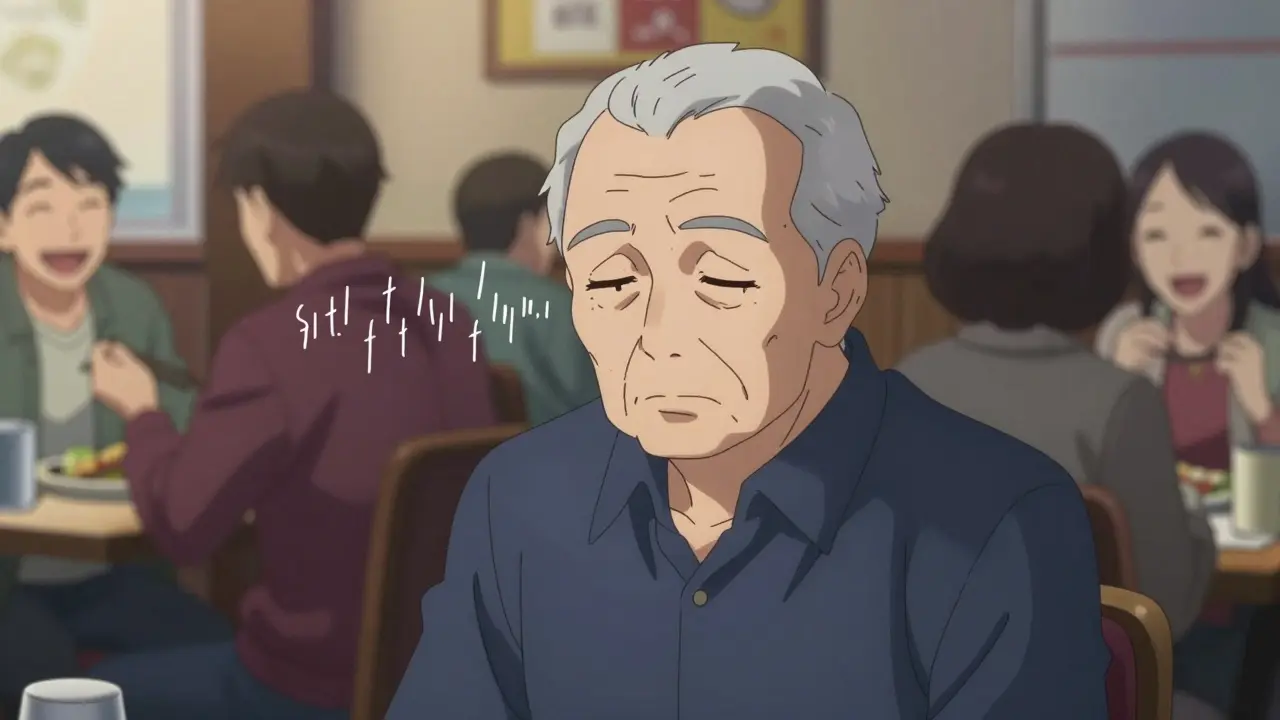
Presbycusis doesn’t hit you all at once. It creeps in slowly. At first, you notice you’re turning up the TV louder than usual. Then you start asking people to repeat themselves, especially when they’re speaking quickly or in a noisy place. You catch yourself nodding along in conversations, pretending you heard what was said. The worst part? You start avoiding social events because it’s exhausting trying to keep up.This isn’t just about volume. It’s about clarity. High-pitched sounds - like children’s voices, birds chirping, or the beeps of a microwave - fade first. Consonants like ‘s,’ ‘th,’ and ‘f’ become muffled. That’s why someone might say, “I’ll see you at three,” but you hear, “I’ll see you at tree.” Speech discrimination drops by 15-30% in people with untreated presbycusis. In quiet rooms, you might manage okay. But in restaurants, family gatherings, or even the doctor’s office, understanding becomes a struggle.
And it’s more than just missing words. Nearly 60% of people with this condition also deal with tinnitus - that constant ringing or buzzing in the ears. One in three adults between 65 and 74 has hearing loss. By 75, it’s nearly half. These aren’t small numbers. They’re millions of people quietly withdrawing from life because they can’t hear it anymore.
Why Your Ears Are Changing
Your inner ear has about 16,000 tiny hair cells that turn sound waves into signals your brain understands. You’re born with all of them - and you don’t grow new ones. Starting around age 30, you lose about 1% per year. That’s not dramatic until you hit your 60s or 70s, when the damage adds up. These cells don’t regenerate. Once they’re gone, they’re gone.Genetics play a big role too. If your parents or grandparents had trouble hearing later in life, you’re more likely to. But environment matters just as much. Years of exposure to loud noises - construction work, concerts, even loud headphones - can speed up the process. Studies show that consistent noise over 85 decibels (about the level of heavy traffic) increases your risk of hearing loss by 40%.
Other health conditions make it worse. Diabetes raises your risk by 28%. High blood pressure adds 23%. Smoking? That’s a 15% increase. These conditions damage blood flow to the inner ear, starving the hair cells of oxygen. It’s not just your ears aging - it’s your whole body.
The Hidden Costs of Ignoring It
Most people think hearing loss is just an inconvenience. It’s not. It’s a silent crisis with real consequences.People with untreated hearing loss are 5.3 times more likely to feel socially isolated. Depression rates jump by 32%. One in four older adults with hearing loss misses important health instructions during doctor visits. That’s not just frustrating - it’s dangerous. You might not know you’re supposed to take your medication twice a day, or that your blood pressure meds need adjusting.
And then there’s the brain. A 2020 Lancet report found untreated hearing loss increases dementia risk by 50%. Why? Because when your brain struggles to process sound, it overworks itself. Over time, this strain may accelerate cognitive decline. Treating hearing loss at 60 instead of 70 could reduce that risk by 8-10% over a decade, according to Johns Hopkins research.
There’s also a financial hit. People with untreated hearing loss earn an average of $30,000 less per year than their peers with normal hearing. That’s not because they’re less capable - it’s because communication problems affect job performance, promotions, and even interviews.

Hearing Aids: The Real Solution
The good news? Hearing aids work. Not perfectly, but well enough to make a huge difference.Modern hearing aids aren’t just tiny speakers that make everything louder. They’re smart computers. They use 16 to 64 frequency channels to boost only the sounds you need - like speech - while reducing background noise. Directional microphones focus on the person talking in front of you, not the clatter from behind. Bluetooth lets you stream phone calls, TV, and music directly to your hearing aids. Some even track your steps or monitor how often you’re socializing.
Studies show properly fitted hearing aids improve speech understanding by 40-60% in quiet settings and 25-40% in noisy ones. Eighty-five percent of users report better communication. But here’s the catch: only 30% of people who need them actually use them.
Why? Cost. Prescription hearing aids cost $1,800 to $3,500 per ear. That’s a lot, especially since Medicare doesn’t cover them (though some Medicare Advantage plans now do, covering over 28 million people as of 2024). But there’s another option: over-the-counter (OTC) hearing aids. Since the FDA opened the market in 2022, OTC devices have surged in popularity. They cost $200-$1,000 per pair. Brands like Jabra Enhance Select and Eargo are popular choices. They’re not as customizable as prescription models, but for mild to moderate hearing loss, they’re a solid, affordable start.
Top-rated prescription models like Oticon More and Widex Moment score above 85 out of 100 in independent reviews. For OTC, Jabra leads with a 78. But the best device is the one you’ll actually wear.
What to Expect - And What to Avoid
If you’re thinking about getting hearing aids, here’s what you need to know:- You won’t hear like you did at 20. Don’t expect perfection. But you’ll hear enough to reconnect with life.
- It takes time. Most people adapt within 4-6 weeks. Some features, like smartphone apps, need 12 hours of practice to master.
- Fitting matters. If your hearing aids feel loose, whistling, or uncomfortable, go back. A good audiologist will adjust them multiple times - at 1, 2, and 4 weeks - until they feel right.
- Wind noise is a common complaint. Look for models with wind-reduction technology if you walk outside often.
- Rechargeable models are becoming standard. They last 16-20 hours per charge and eliminate the hassle of tiny batteries.
- Don’t skip the trial. Most clinics offer a 30-60 day trial. Use it. If it’s not working, return it.
And avoid the trap of waiting. The longer you delay, the harder it becomes for your brain to relearn how to process sound. That’s why experts like Dr. Gayla Poling at Mayo Clinic say: “Modern hearing aids aren’t just amplifiers - they’re brain trainers.”
What You Can Do Today
You don’t need to wait for a crisis to act.- If you’re 50 or older, get a baseline hearing test. It’s quick, painless, and often free at audiology clinics.
- Get screened every two years after that.
- Ask your doctor if they check your hearing during routine visits. Most don’t - but you can request it.
- If you’re already using hearing aids and they’re not helping, don’t give up. Go back. Technology has improved drastically in the last five years. Your old model might be outdated.
- Use assistive tools: captioned TV, amplified phones, or apps like Beltone’s SoundClear that test your hearing at home.
One Reddit user, HearingHopeful42, wrote: “After 15 years of pretending to hear, my Phonak Audeo M-312s restored my ability to hear my granddaughter’s laughter clearly.” That’s not just a happy ending - it’s a common one.
Hearing loss doesn’t have to mean silence. With the right tools and the right timing, you can stay connected, safe, and engaged - no matter your age.
Is presbycusis the same as general hearing loss?
Presbycusis is a specific type of hearing loss caused by aging. It’s sensorineural, meaning it comes from damage to the inner ear’s hair cells or the nerve pathways to the brain. Not all hearing loss is presbycusis - noise-induced, medication-related, or earwax blockage can also cause hearing problems. But if you’re over 60 and noticing trouble with high-pitched sounds and speech in noise, it’s most likely presbycusis.
Can hearing aids restore my hearing to normal?
No, hearing aids can’t restore hearing to what it was when you were younger. But they can restore your ability to understand speech, enjoy conversations, and participate in daily life. Most users report a 40-60% improvement in quiet settings and 25-40% in noisy ones. The goal isn’t perfection - it’s connection.
Are over-the-counter hearing aids any good?
Yes - for mild to moderate hearing loss. OTC hearing aids, approved by the FDA since 2022, are a legitimate, affordable option. Brands like Jabra Enhance Select and Eargo are well-reviewed. They’re not as customizable as prescription devices and won’t help with severe loss, but for many people, they’re a great first step. If they don’t work, you can always upgrade later.
Why do some people stop using their hearing aids?
The top reasons are poor fit (45%), discomfort (30%), and not hearing well in noisy places (25%). Many people get a device and expect instant results. But hearing aids need time to adjust - both the device and your brain. A good audiologist will fine-tune the settings over several visits. If you’re unhappy, go back. Don’t give up after one try.
Can hearing loss lead to dementia?
Untreated hearing loss is linked to a 50% higher risk of dementia, according to the 2020 Lancet Commission. The theory is that when your brain works overtime trying to decode sounds, it has less capacity for memory and thinking. Treating hearing loss early may slow this decline. Studies suggest starting treatment at 60 instead of 70 could reduce dementia risk by 8-10% over ten years.
How often should I get my hearing checked?
If you’re 50 or older, get a baseline test. After that, have your hearing checked every two years. If you notice sudden changes - like trouble hearing one ear, ringing, or dizziness - see a specialist right away. Regular screenings catch problems early, when they’re easiest to manage.


13 Comments
Ian Long
January 9, 2026 AT 18:02I used to think hearing aids were for old folks who couldn’t keep up. Then I started missing my kid’s jokes at dinner. Now I wear mine daily and actually laugh again. Best $800 I ever spent.
Angela Stanton
January 11, 2026 AT 03:33Let’s be real - the FDA’s OTC mandate was a corporate power grab disguised as consumer empowerment. 78% user satisfaction? That’s statistically meaningless without audiometric validation. You’re trading clinical precision for Amazon Prime delivery. And don’t get me started on the lack of real-time noise floor calibration in these budget devices. 🤦♀️
Johanna Baxter
January 11, 2026 AT 23:05I’m 68 and I refuse to wear a hearing aid. My husband says I’m just being stubborn but I’ve had enough of people telling me what’s wrong with me. I’ll keep nodding and smiling. It’s easier than listening to everyone’s opinions on my ears. 😒
Jerian Lewis
January 13, 2026 AT 16:17It’s not just the hair cells. It’s the neural plasticity decay. Your brain forgets how to filter signal from noise when it hasn’t had the input for years. That’s why even perfect hearing aids feel ‘off’ after decades of neglect. The tech isn’t broken - your cortex is.
Kiruthiga Udayakumar
January 13, 2026 AT 19:42Why is everyone so obsessed with buying gadgets? In India, we just sit closer, speak slower, and hold hands while talking. Technology doesn’t fix loneliness. Connection does. 🙏
Patty Walters
January 14, 2026 AT 03:55Got my first OTCs last year - Jabra Enhance. Took 3 weeks to get used to them, but now I hear my cat purr from the other room. Honestly? I thought I was just getting old. Turns out I was just deaf. 😅
Phil Kemling
January 15, 2026 AT 22:54If we accept aging as inevitable, why do we treat hearing loss like a failure? We don’t blame people for gray hair. Why do we shame them for missing the ‘s’ in ‘cats’? Maybe the problem isn’t the ears - it’s our obsession with perfect auditory performance in a noisy world.
Maggie Noe
January 17, 2026 AT 02:45My grandma wore hearing aids for 12 years and still asked me to repeat myself every 30 seconds. I’m not saying they don’t help - I’m saying they’re not magic. And the whistling? The feedback? The battery anxiety? 😭 I’d rather just yell.
Gregory Clayton
January 18, 2026 AT 19:11They want you to buy these $3K devices because they know you’re too lazy to just turn the TV up. This whole ‘presbycusis crisis’ is just Big Hearing trying to sell you a subscription. We used to live fine without all this tech. Now we’re drowning in gadgets.
Catherine Scutt
January 18, 2026 AT 23:28Why do people still think OTC aids are okay? If you can’t afford a real audiologist, you’re not ready for a hearing aid. You’re ready for a reality check. And if you’re using them to avoid social interaction? That’s not a fix - that’s a cop-out.
Darren McGuff
January 20, 2026 AT 07:41As an audiologist of 27 years, I’ve seen the shift. OTC devices are a gateway - not a replacement. People who buy them often return within 6 months for proper fitting. That’s not failure. That’s progress. The real win? They’re finally asking for help.
Alicia Hasö
January 20, 2026 AT 16:27To anyone hesitating: Your silence isn’t protecting your dignity - it’s stealing your joy. The first time you hear your grandchild say ‘I love you’ clearly? That’s worth every awkward adjustment. You’re not broken. You’re just overdue for an upgrade.
Ashley Kronenwetter
January 21, 2026 AT 13:17Thank you for writing this with such clarity. I’ve shared it with my mother, who’s been avoiding testing for five years. I hope this is the nudge she needs.