Diuretics Explained – What They Are and How They Work
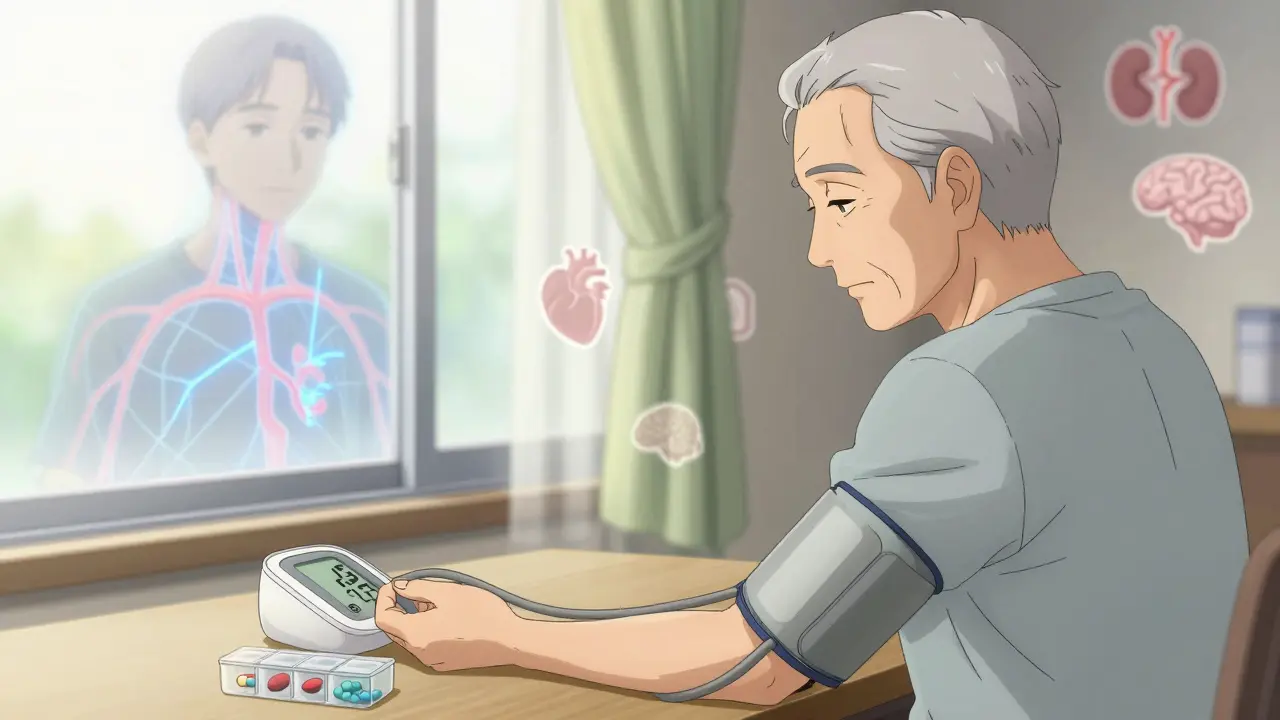
If you've ever heard a doctor mention "water pills," they're talking about diuretics. These meds help your body get rid of extra fluid by making you pee more often. The result is less swelling, lower blood pressure, and easier breathing for some conditions.
Diuretics work on the kidneys, which filter waste and control how much water stays in your bloodstream. By tweaking that balance, they pull out sodium and water, sending it straight to the bathroom. It sounds simple, but each type does it a little differently, so knowing the basics can save you headaches later.
Why People Take Diuretics
Most folks need diuretics for three big reasons: swelling (edema), high blood pressure (hypertension), and certain heart or kidney problems. If your ankles puff up after a long flight, a doctor might prescribe a low‑dose diuretic to shrink that fluid. For hypertension, getting rid of excess water eases the pressure on artery walls, which can lower the risk of strokes.
Some athletes also use them to cut weight quickly, but that's risky and usually illegal in sports. The key takeaway? Diuretics are not a one‑size‑fits‑all solution; they target specific issues where fluid buildup is a problem.
Common Types and What to Watch For
The three main families are thiazide, loop, and potassium‑sparing diuretics. Thiazides (like hydrochlorothiazide) are often the first pick for blood pressure because they’re gentle and cheap. Loop diuretics (such as furosemide) are stronger and used when there’s a lot of fluid, like in heart failure.
Potassium‑sparing pills (spironolactone is a popular one) keep your potassium levels from dropping too low—a common side effect of the other two types. Speaking of side effects, watch for frequent urination, dizziness, or muscle cramps. Low potassium can cause weakness and irregular heartbeats, so many doctors will check blood labs after you start a diuretic.
Always tell your pharmacist about any other meds, especially NSAIDs or certain antidepressants, because they can mess with how diuretics work. And if you feel unusually thirsty, light‑headed, or notice swelling coming back, give your doctor a call—adjustments might be needed.
Bottom line: diuretics are handy tools for controlling fluid and blood pressure, but they need careful use. Stick to the prescribed dose, keep an eye on how you feel, and get regular check‑ups. With the right approach, water pills can help you stay comfortable and healthier without unwanted surprises.
Blood Pressure Medications: Types, Side Effects, and Safety
Learn the four main types of blood pressure medications, their side effects, and how to stay safe while taking them. Understand why some drugs work better for certain people and how to stick with your treatment plan.
Lasix Alternatives: Effective Diuretic Options for Heart Failure Treatment
Heart failure can be overwhelming, but managing the fluid overload doesn't have to be stuck on Lasix alone. This guide explores real-world alternatives to Lasix, their pros and cons, and how doctors personalize treatment for congestive heart failure. Get clear, practical tips about diuretic options and lifestyle changes to help your heart work less and you live more comfortably. Learn what truly matters in day-to-day management beyond the usual prescription.
© 2026. All rights reserved.