When someone is diagnosed with cancer, one of the first things they hear is that chemotherapy might be part of their treatment. It’s not just a buzzword-it’s a powerful tool that’s saved millions of lives since the 1940s. But chemotherapy isn’t simple. It doesn’t just attack cancer. It hits fast-growing cells everywhere, including your hair follicles, gut lining, and bone marrow. And when you’re taking other medications-prescription, over-the-counter, or even supplements-the risks multiply. Drug interactions can turn a life-saving treatment into a dangerous one.
How Chemotherapy Works and Why It’s Still Essential
Chemotherapy uses chemicals to kill cancer cells by targeting their ability to divide and multiply. Unlike surgery or radiation, which are local, chemo works systemically. That means it can reach cancer that’s spread beyond its original site. About 650,000 people in the U.S. get chemotherapy each year, and more than half of all cancer patients will receive it at some point.
There are over 100 different chemo drugs, grouped into classes based on how they work. Anthracyclines like doxorubicin damage DNA directly but can harm the heart if used too long-doctors limit total lifetime doses to 450-550 mg/m². Alkylating agents like cyclophosphamide cross-link DNA strands. Antimetabolites like methotrexate mimic building blocks of DNA, tricking cells into using the wrong material. Plant alkaloids like vincristine freeze cell division machinery.
Most patients don’t get just one drug. Combination regimens-like BEP for testicular cancer or AC-T for breast cancer-are standard because they attack cancer in multiple ways at once. This reduces the chance of resistance. The science behind it? The fraction kill hypothesis: each dose kills a fixed percentage of cancer cells, no matter how big the tumor is. That’s why cycles repeat every 2-4 weeks: to let healthy cells recover while keeping pressure on the cancer.
Why Drug Interactions Are a Silent Threat
Chemotherapy doesn’t live in a vacuum. Most cancer patients are also taking meds for other conditions-high blood pressure, diabetes, depression, acid reflux. Even something as simple as St. John’s wort or grapefruit juice can interfere.
Many chemo drugs are broken down by liver enzymes, especially CYP3A4 and CYP2D6. If another drug blocks or speeds up these enzymes, chemo levels can spike or drop dangerously. For example, ketoconazole (an antifungal) can slow the breakdown of paclitaxel, leading to toxic buildup. On the flip side, rifampin (used for TB) can make chemo less effective by speeding up its metabolism.
Even common pain relievers matter. NSAIDs like ibuprofen can increase bleeding risk when paired with drugs like cisplatin, which already lower platelet counts. Acetaminophen is safer, but high doses can stress the liver-already under pressure from chemo. And don’t forget supplements. Vitamin C in high doses may interfere with doxorubicin. Omega-3s can thin the blood. Turmeric? It affects drug metabolism pathways too.
A 2023 study in the Journal of Clinical Oncology found that nearly 40% of cancer patients on chemo were taking at least one medication with a known or potential interaction. One in five had a moderate to high-risk interaction. Many patients didn’t even know their supplements could be dangerous.
Real-World Consequences: When Interactions Go Wrong
Interactions aren’t theoretical. They cause real harm.
In one case, a 58-year-old woman with ovarian cancer was prescribed oral cyclophosphamide and started taking omeprazole for heartburn. Omeprazole inhibits CYP2C19, the enzyme needed to activate cyclophosphamide. Her treatment failed. The cancer progressed. She later learned that pantoprazole would have been a safer acid reducer.
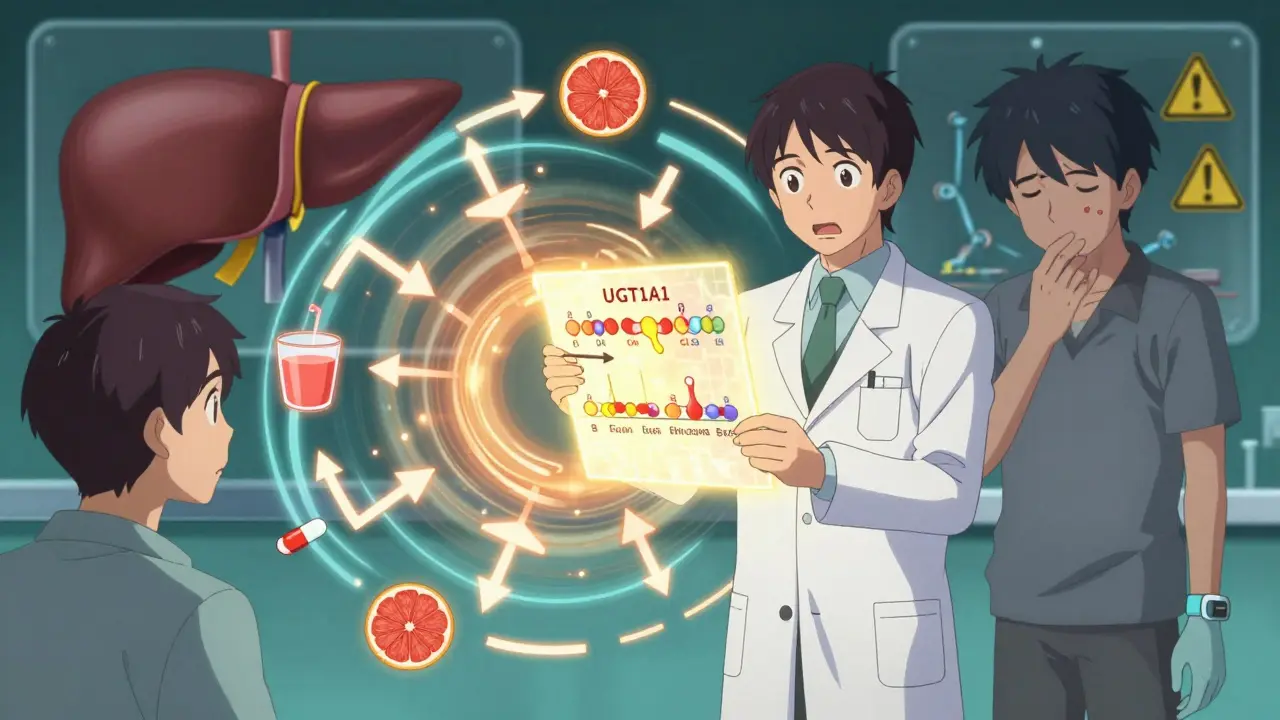
Another patient, on irinotecan for colon cancer, developed severe diarrhea after starting a new statin. Irinotecan is processed by UGT1A1. Some people have a genetic variant that slows this down, making them more sensitive. The statin worsened the effect. Genetic testing for UGT1A1 is now standard before starting irinotecan-but not everyone gets it.
Even antibiotics can be risky. Fluoroquinolones like ciprofloxacin can increase the risk of tendon rupture when combined with corticosteroids, which are often given with chemo to reduce inflammation. And if you’re on warfarin for atrial fibrillation, chemo can make your INR swing wildly-leading to clots or bleeding.
The bottom line: every medication, every supplement, every herb-needs to be on the table. Not just the ones you think matter.
Who’s at Highest Risk?
Not everyone faces the same level of risk. Certain groups are more vulnerable:
- Older adults: Often on multiple meds for chronic conditions. Kidney and liver function decline with age, slowing drug clearance.
- Patients with liver or kidney disease: These organs clear chemo drugs. If they’re not working well, drugs build up.
- Those on multiple drugs: The more meds you take, the higher the chance of interaction. Five or more medications? Risk jumps significantly.
- People using complementary therapies: Herbal supplements, vitamins, CBD-many aren’t studied in cancer patients. They’re assumed safe, but they’re not.
- Patients with genetic variations: CYP2D6, UGT1A1, DPYD-these genes affect how you process drugs. Testing isn’t universal, but it should be for key agents.
Black patients are disproportionately affected. A 2023 Patient Advocacy Foundation report showed they were 1.7 times more likely to have chemotherapy delayed due to low white blood cell counts. Part of that is access, but part is also less frequent use of genetic testing and supportive care to prevent toxicity.
What You Can Do: A Practical Guide
You don’t have to be a scientist to protect yourself. Here’s what actually works:
- Make a full list. Write down every pill, patch, capsule, drop, and herbal tea you take. Include doses and how often. Don’t leave anything out-not even aspirin or melatonin.
- Bring it to every appointment. Show it to your oncologist, pharmacist, and nurse. Don’t assume they know what you’re taking. Many patients forget to mention supplements.
- Ask two questions: "Can this interact with my chemo?" and "Is there a safer alternative?" If they don’t know, ask for a pharmacist consult.
- Use one pharmacy. If you get prescriptions from different doctors, use one pharmacy. They can flag interactions across all your meds.
- Check before you buy. Before taking any new OTC drug or supplement, ask your oncology team. Even "natural" doesn’t mean safe.
- Know your genetics. If you’re getting irinotecan, ask about UGT1A1 testing. If you’re on tamoxifen, ask about CYP2D6. These tests are simple, cheap, and can prevent serious side effects.
Some hospitals now use electronic systems that flag interactions automatically. But not all do. If yours doesn’t, you have to be your own advocate.

The Future: Safer Chemotherapy
Science is catching up. Newer drugs are designed to avoid these problems. Antibody-drug conjugates like sacituzumab govitecan (Trodelvy) deliver chemo directly to cancer cells, reducing exposure to healthy tissue. That means fewer interactions and fewer side effects.
Circulating tumor DNA (ctDNA) testing is also changing things. Instead of giving chemo for a fixed number of cycles, doctors can now test blood to see if cancer is still present. If not, they stop. A 2023 trial showed this cut unnecessary chemo by 32% in colon cancer patients-meaning fewer chances for drug interactions altogether.
And pharmacogenomics is becoming standard. Before giving certain chemo drugs, labs now routinely check for gene variants that predict toxicity. It’s not perfect yet-but it’s moving fast.
Still, chemotherapy isn’t going away. It’s still the backbone of curative treatment for most cancers. The goal isn’t to replace it-it’s to make it smarter, safer, and more personalized.
Final Thoughts: Your Power in This Process
Chemotherapy is intense. The fatigue, the nausea, the hair loss-it’s a lot. But the biggest danger isn’t always the chemo itself. It’s what you’re taking alongside it.
You don’t need to memorize drug names or enzyme pathways. You just need to be organized and speak up. Keep a list. Ask questions. Don’t be shy. Your oncology team wants you to survive-not just live, but live well.
And remember: if something feels off-unusual fatigue, strange bruising, sudden nausea, numbness in your hands or feet-tell someone. Early intervention can stop a small problem from becoming a life-threatening one.
Chemotherapy saved lives. But it’s not magic. It’s medicine. And medicine works best when it’s managed with care, clarity, and communication.
Can I take over-the-counter pain relievers while on chemotherapy?
It depends. Acetaminophen (Tylenol) is generally safe in standard doses. Avoid NSAIDs like ibuprofen or naproxen if your chemo lowers platelets or affects kidney function-they can increase bleeding risk. Always check with your oncology team before taking anything, even something as simple as aspirin.
Do herbal supplements interfere with chemotherapy?
Yes, many do. St. John’s wort can reduce the effectiveness of drugs like doxorubicin and cyclophosphamide. Turmeric, green tea extract, and high-dose vitamin C may interfere with chemo’s ability to kill cancer cells. Even melatonin and omega-3s can affect blood clotting. Never assume "natural" is safe-always disclose everything you take.
Why do I need genetic testing before some chemo drugs?
Some people have genetic variations that affect how their body processes chemo. For example, UGT1A1*28 increases the risk of severe diarrhea from irinotecan. CYP2D6 variants can make tamoxifen ineffective. Testing helps doctors choose the right dose or avoid the drug entirely, preventing life-threatening side effects.
Can grapefruit juice affect my chemotherapy?
Yes. Grapefruit juice blocks an enzyme called CYP3A4 in the gut, which can cause certain chemo drugs-like docetaxel, etoposide, and vinca alkaloids-to build up to toxic levels. Even one glass can have an effect for days. Avoid it completely during treatment unless your oncologist says it’s safe.
What should I do if I start a new medication while on chemo?
Stop. Don’t take it. Call your oncology team immediately. Even if it’s prescribed by another doctor, they need to check for interactions with your chemo regimen. Many hospitals have oncology pharmacists on staff specifically for this purpose-use them.
How can I make sure my pharmacy catches potential interactions?
Use one pharmacy for all your prescriptions-including chemo, pain meds, and supplements. Tell them you’re on chemotherapy and ask them to flag any potential interactions. Many pharmacies have systems that catch these, but only if they know your full medication list. Don’t assume they’ll know-tell them.
Are there any chemo drugs that are safer with fewer interactions?
Newer agents like antibody-drug conjugates (e.g., Trodelvy) deliver chemo directly to cancer cells, reducing exposure to the rest of the body. This lowers the chance of interactions with other drugs. But even these aren’t risk-free. The safest approach is always personalized treatment based on your full health picture-not just the drug.
Next steps: Start today. Write down every medication and supplement you take. Bring that list to your next appointment. Ask your oncologist if you need genetic testing. Don’t wait for a problem to happen-prevent it before it starts.


13 Comments
Jake Moore
January 17, 2026 AT 14:01Just wanted to say this post is a game-changer. I’ve been on chemo for 18 months and didn’t realize how many of my ‘harmless’ supplements were throwing off my drug levels. Started cutting out turmeric and green tea after reading this-my ANC went up within two weeks. If you’re on chemo, treat your meds like a bomb squad checklist. No exceptions.
Naomi Keyes
January 19, 2026 AT 10:40Actually, I think this article underestimates the systemic negligence in oncology care-especially regarding pharmacogenomics. Why are we still relying on patient self-reporting when we have $200 SNP panels that could prevent 60% of toxicities? Hospitals aren’t mandated to test for UGT1A1 or DPYD before prescribing irinotecan or 5-FU-this isn’t oversight, it’s malpractice disguised as cost-cutting.
Nishant Sonuley
January 20, 2026 AT 09:33Man, I love how this post breaks it down without sugarcoating-but also without fearmongering. I’m from India, and here, people take ashwagandha, turmeric, and a dozen other ‘Ayurvedic’ pills alongside chemo like it’s tea. No one tells them it’s like pouring gasoline on a fire. I’ve seen patients crash from liver toxicity because their ‘natural’ remedies were blocking CYP3A4. This needs to be translated into ten languages and posted in every clinic waiting room. Seriously.
Zoe Brooks
January 21, 2026 AT 16:28This is why I always say: your oncologist isn’t your only doctor-you’re the CEO of your own treatment. 🙌 Keep the list. Ask the questions. Say ‘I need to check with my pharmacist’ like it’s your superpower. You got this.
Praseetha Pn
January 21, 2026 AT 20:09Oh, so now we’re blaming supplements? Let me guess-Big Pharma wants you to stop taking anything that’s not patented, right? Turmeric’s been used for 4,000 years. Vitamin C? It’s a natural antioxidant-how is that dangerous unless you’re being paid to sell you more chemo? And don’t get me started on ‘genetic testing’-they’re just trying to monetize your DNA now. You think they care if you live? They care if you keep paying for scans.
Stacey Marsengill
January 22, 2026 AT 08:09I’ve been through this. Twice. And let me tell you-when your platelets hit 8,000 because you took ibuprofen for a headache, you don’t just ‘learn a lesson.’ You learn what it feels like to be a statistic. I didn’t even know I was on warfarin until the ER nurse screamed, ‘Who gave you NSAIDs?!’ I’m alive because I screamed back. Don’t be polite. Be loud. Be annoying. Your life isn’t a polite conversation.
Emma #########
January 23, 2026 AT 19:29Thank you for writing this. My mom just started chemo and I’ve been her medication manager since day one. I printed out the list of interactions and laminated it. We take it to every appointment. I wish more people understood how much power they have just by being organized.
rachel bellet
January 24, 2026 AT 09:28It’s not just about the drugs-it’s about the arrogance of the medical system. We assume patients are ignorant, so we don’t educate them. We assume they’ll forget, so we don’t document. We assume they’ll ‘just know’ to avoid grapefruit juice, but we don’t even put it on the discharge papers. The real danger isn’t the interaction-it’s the institutional indifference. This post is a bandage on a hemorrhage.
Max Sinclair
January 25, 2026 AT 03:32One thing this article doesn’t emphasize enough: pharmacists are your secret weapon. Most oncology clinics have a dedicated oncology pharmacist on staff-use them. They don’t just fill prescriptions; they audit your entire regimen for interactions, contraindications, and dosing pitfalls. If your clinic doesn’t have one, ask why. And if they say, ‘We don’t have funding,’ tell them your life is worth more than their budget.
Andrew McLarren
January 25, 2026 AT 17:31While the clinical information presented is both accurate and commendable, I must respectfully underscore the ethical imperative of patient autonomy in this context. The onus of vigilance should not rest solely upon the individual, particularly given the cognitive and emotional burdens imposed by cancer therapy. A systemic, institutionalized approach-mandating pre-chemotherapy pharmacogenomic screening and centralized medication reconciliation-is not merely advisable; it is a moral obligation.
Ryan Otto
January 26, 2026 AT 16:23Let’s be honest: chemotherapy is a blunt instrument designed by corporations who profit from repeated cycles. The ‘interactions’ they warn you about? They’re the same companies that suppress research on natural compounds that could replace chemo. They need you dependent. They need you confused. They need you believing that your turmeric is the enemy-not their profit margins. This post reads like a pharmaceutical pamphlet. Don’t be fooled.
Andrew Short
January 28, 2026 AT 07:08Of course you’re supposed to ‘ask questions.’ But how many patients actually get listened to? I’ve seen oncologists roll their eyes when patients bring up supplements. They don’t want to hear it-they want compliance. And if you’re not white, middle-class, and insured? Good luck getting genetic testing. This whole thing is a privilege. Don’t pretend it’s not.
christian Espinola
January 29, 2026 AT 17:04Just one sentence: Stop taking anything not prescribed by your oncologist. Period.