Antibiotic Decision Aid
Select Your Situation
This tool helps identify appropriate antibiotic options based on your specific health situation and infection type.
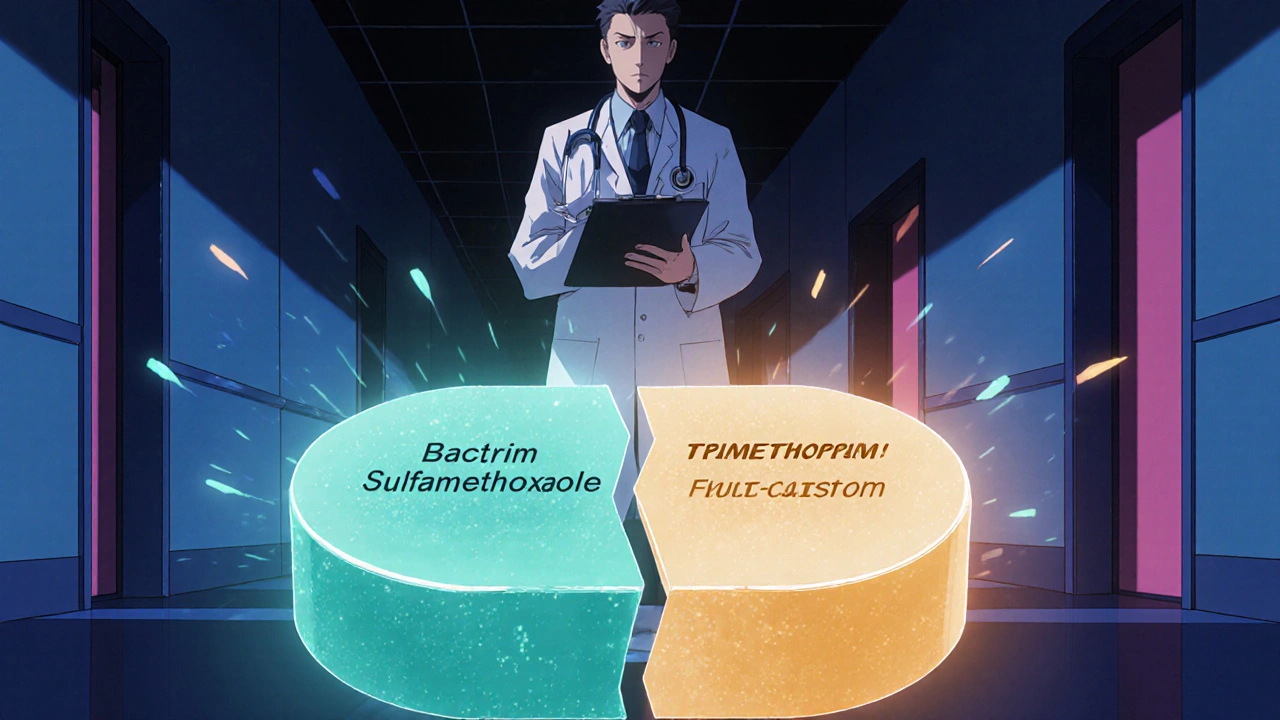
When doctors write a prescription for Bactrim (sulfamethoxazole/trimethoprim), most patients wonder what they’re actually taking and whether another pill might work just as well. Below you’ll find a straightforward, side‑by‑side look at Bactrim and the most frequently used alternatives, so you can decide what makes sense for your infection, health history, and lifestyle.
Key Takeaways
- Bactrim combines two drugs to block bacterial folic‑acid production, making it great for urinary‑tract infections (UTIs) and certain respiratory bugs.
- Common alternatives-doxycycline, azithromycin, amoxicillin‑clavulanate, nitrofurantoin, and cefuroxime-differ in spectrum, dosing ease, and safety in pregnancy.
- Side‑effect profiles vary: Bactrim can trigger kidney concerns; doxycycline may cause sun sensitivity; azithromycin is usually gentle on the gut.
- Pick an antibiotic based on infection type, local resistance trends, drug interactions, and personal factors like pregnancy or kidney disease.
- Always finish the full course, even if you feel better, to prevent resistance.
Bactrim comparison starts with understanding the drug itself.
What Is Bactrim?
Bactrim (Sulfamethoxazole/Trimethoprim) is a fixed‑dose combination antibiotic that pairs sulfamethoxazole, a sulfonamide, with trimethoprim, a dihydrofolate‑reductase inhibitor. This duo blocks two steps in the bacterial folic‑acid pathway, delivering a double‑hit that many single agents can’t match.
Originally approved in 1971, Bactrim quickly became a go‑to for uncomplicated urinary‑tract infections, some forms of pneumonia (especially caused by Legionella), and certain skin infections. In Canada and the U.S., it’s sold under the brand name Bactrim and generics like Septra.
How Bactrim Works
Both components act on the same metabolic chain but at different points. Sulfamethoxazole mimics para‑aminobenzoic acid (PABA) and competitively inhibits dihydropteroate synthase, while trimethoprim blocks dihydrofolate reductase. The result? Bacteria can’t make the folic acid they need for DNA synthesis, so they stop growing.
This synergistic mechanism gives Bactrim a broader spectrum than either drug alone and helps lower the chance of resistance-provided you use it correctly.
When Doctors Prescribe Bactrim
- Uncomplicated urinary‑tract infections (UTIs) in adults
- Acute bacterial sinusitis (when other options aren’t suitable)
- Community‑acquired pneumonia caused by atypical organisms
- Skin and soft‑tissue infections like impetigo
- Prophylaxis for certain opportunistic infections in immunocompromised patients
Typical Dosage and Duration
For most adult UTIs, the standard dose is one double‑strength tablet (800 mg sulfamethoxazole + 160 mg trimethoprim) every 12 hours for 3 days. For respiratory infections, dosing may extend to 5-7 days.
Side Effects and Contra‑Indications
While many tolerate Bactrim well, it can cause:
- Skin rash or photosensitivity (especially in people with sulfa allergies)
- Gastro‑intestinal upset - nausea, vomiting
- Kidney‑related issues - rise in creatinine, especially in those with existing renal impairment
- Rare but serious blood abnormalities - agranulocytosis, Stevens‑Johnson syndrome
It’s contraindicated in:
- Pregnant women in the first trimester (risk of neural‑tube defects)
- Patients with severe sulfonamide allergy
- Severe renal or hepatic disease without dose adjustment
Top Antibiotic Alternatives
Below are the most commonly considered substitutes when Bactrim isn’t appropriate.
Doxycycline is a tetracycline‑class antibiotic that inhibits bacterial protein synthesis by binding to the 30S ribosomal subunit
Doxycycline is broad‑spectrum, covering many gram‑positive and gram‑negative bacteria, as well as atypical pathogens like Mycoplasma. It’s often chosen for acne, Lyme disease, and as a backup for atypical pneumonia.
Typical adult dose: 100 mg twice daily for 7-14 days. Main downsides: photosensitivity, nausea, and it can’t be used in children under eight or pregnant women.
Azithromycin is a macrolide antibiotic that blocks bacterial protein synthesis by attaching to the 50S ribosomal subunit
Azithromycin’s long half‑life allows once‑daily dosing, often for 3 days, making it popular for community‑acquired pneumonia, chlamydia, and certain skin infections.
Side effects are usually mild-diarrhea, mild liver enzyme elevation-but it can interact with drugs that affect the QT interval.
Amoxicillin‑Clavulanate is a beta‑lactam/beta‑lactamase inhibitor combo that expands amoxicillin’s activity against beta‑lactamase‑producing bacteria
This combo hits many respiratory pathogens, sinus infections, and some urinary‑tract bugs. It’s a solid choice when you need a broader gram‑negative cover than plain amoxicillin.
Standard adult dose: 875 mg/125 mg twice daily for 7-10 days. Notable side effects: GI upset and a higher chance of diarrhea compared with amoxicillin alone.
Nitrofurantoin is a nitrofuran‑type antibiotic that is reduced by bacterial enzymes to reactive metabolites that damage bacterial DNA
Nitrofurantoin is a urine‑concentrating drug, making it a first‑line option for uncomplicated UTIs, especially in women.
Dosage: 100 mg twice daily for 5 days. It’s safe in pregnancy (after the first trimester) but should be avoided in patients with poor kidney function.
Cefuroxime is a second‑generation cephalosporin that interferes with bacterial cell‑wall synthesis
Useful for sinusitis, bronchitis, and some skin infections, cefuroxime offers a broader gram‑negative coverage than first‑generation cephalosporins.
Typical dose: 250-500 mg twice daily for 7-10 days. It’s generally well‑tolerated, though people with penicillin allergy may react.
Side‑by‑Side Comparison Table
| Antibiotic | Spectrum | Typical Indications | Dosage Frequency | Pregnancy Safety | Common Side Effects |
|---|---|---|---|---|---|
| Bactrim (SMX/TMP) | Broad (Gram‑+, Gram‑‑, some atypicals) | UTI, atypical pneumonia, skin infections | Every 12 h | Contra‑indicated 1st trimester | Rash, kidney impact, GI upset |
| Doxycycline | Broad, good for atypicals | Acne, Lyme, atypical pneumonia | Twice daily | Contra‑indicated (pregnancy, <8 y) | Photosensitivity, nausea |
| Azithromycin | Moderate, targets respiratory bugs | Pneumonia, chlamydia, skin | Once daily (3 d) | Generally safe | Diarrhea, QT prolongation risk |
| Amoxicillin‑Clavulanate | Broad, beta‑lactamase resistant | Sinusitis, otitis, some UTIs | Twice daily | Safe (all trimesters) | GI upset, diarrhea |
| Nitrofurantoin | UTI‑focused (urine‑concentrated) | Uncomplicated cystitis | Twice daily | Safe after 1st trimester | Pulmonary toxicity (rare), GI |
| Cefuroxime | Broad gram‑negative/positive | Sinusitis, bronchitis, skin | Twice daily | Safe (all trimesters) | Allergic reactions, mild GI |
How to Choose the Right Antibiotic
Think of picking an antibiotic like matching a lock to a key. You need to know three things first:
- The bug you’re fighting. Lab cultures are ideal, but doctors often rely on typical patterns (e.g., E. coli for most UTIs).
- Patient factors. Age, kidney function, pregnancy status, and allergy history can push you toward one option over another.
- Local resistance data. Some regions report high resistance to sulfonamides, making doxycycline or nitrofurantoin a safer bet.
Apply these criteria:
- If you have a confirmed E. coli UTI and normal kidney function, Bactrim or nitrofurantoin are both solid. Choose nitrofurantoin if you’re pregnant after the first trimester.
- For a respiratory infection where atypical organisms are suspected, azithromycin or doxycycline often beat Bactrim in terms of dosing convenience.
- When a patient has a sulfa allergy, skip Bactrim entirely-go with doxycycline or a beta‑lactam alternative.
Practical Tips for Patients on Antibiotics
- Take the full course. Even if symptoms fade, stopping early can let resistant bacteria survive.
- Stay hydrated. This helps kidneys clear drugs like Bactrim and nitrofurantoin.
- Watch for warning signs. Severe rash, persistent diarrhea, or sudden fever could mean a serious reaction.
- Mind drug interactions. Bactrim can raise levels of certain blood thinners; azithromycin may affect heart rhythm meds.
- Ask about probiotics. A short probiotic course can soften gut upset, especially with broad‑spectrum agents.
Frequently Asked Questions
Can I take Bactrim if I’m allergic to penicillin?
Yes, because Bactrim contains a sulfonamide, not a beta‑lactam. However, if you have a sulfa allergy, you should avoid it.
Why might my doctor choose nitrofurantoin over Bactrim for a cystitis?
Nitrofurantoin concentrates in urine and has a low impact on gut flora, reducing side‑effects. It also bypasses the kidney‑related concerns that Bactrim can raise.
Is it safe to use azithromycin during the first trimester of pregnancy?
Azithromycin is classified as pregnancy category B, meaning animal studies show no risk and there are no well‑controlled human studies. It’s generally considered safe when benefits outweigh risks.
What should I do if I develop a rash while on Bactrim?
Stop the medication immediately and contact your healthcare provider. A rash could signal a mild allergy or, in rare cases, a severe reaction like Stevens‑Johnson syndrome.
How long does resistance to Bactrim typically develop?
Resistance can emerge after repeated or inappropriate use. Regional surveillance shows rising sulfonamide resistance in some UTI pathogens, which is why culture‑guided therapy is ideal.
Armed with this side‑by‑side view, you can talk to your prescriber confidently, understand why a certain drug is chosen, and know what to watch for while you heal.


10 Comments
Drew Waggoner
October 18, 2025 AT 17:06Bactrim’s double‑hit can feel like a double‑edged sword for patients who are already on multiple meds.
Mike Hamilton
October 18, 2025 AT 17:23I think Bactrim is a good option but its side effect like rashes can be a problem for some, especially if they have sulfa alergy.
Alex Lineses
October 18, 2025 AT 17:40From a pharmacodynamic perspective, the synergistic inhibition of dihydropteroate synthase and dihydrofolate reductase creates a broader antibacterial spectrum than monotherapy.
For clinicians, this means a single regimen can cover both gram‑positive and gram‑negative pathogens, simplifying stewardship protocols.
Nevertheless, patient‑specific factors such as renal clearance and sulfa hypersensitivity must guide selection to avoid iatrogenic harm.
Norman Adams
October 18, 2025 AT 17:56Oh great, another combination pill to make our lives more complicated – because nothing says “precision medicine” like a two‑for‑one deal that forces you to memorize extra side‑effects.
Margaret pope
October 18, 2025 AT 18:13Bactrim works well for UTIs and some pneumonias but watch out for kidney issues especially in older patients it can be tough on the gut too
Karla Johnson
October 18, 2025 AT 18:30When you dive into the comparative landscape of antibiotics, the narrative that emerges is one of nuanced trade‑offs rather than simplistic hierarchies. Bactrim offers a broad spectrum by targeting two separate steps in folic‑acid synthesis, which can be advantageous in mixed infections. However, its sulfonamide component introduces a risk profile that includes hypersensitivity reactions, especially in patients with a known sulfa allergy. Doxycycline, on the other hand, provides excellent coverage for atypical pathogens and is often favored for community‑acquired pneumonia or tick‑borne illnesses. The downside is its photosensitivity, which can be a real inconvenience for patients who spend time outdoors. Azithromycin shines with its convenient once‑daily dosing and short course, making adherence easier for busy individuals. Yet, clinicians must be vigilant about its potential QT‑prolongation and drug–drug interactions. Amoxicillin‑clavulanate stands out for its beta‑lactamase inhibition, expanding its utility against resistant strains, but gastrointestinal upset is a common complaint. Nitrofurantoin remains the gold standard for uncomplicated urinary tract infections due to its high urinary concentrations, though it is contraindicated in patients with impaired renal function. Cefuroxime offers a solid middle ground with decent gram‑negative coverage and tolerability, yet it may not be sufficient for certain resistant organisms. Ultimately, the decision hinges on infection site, patient comorbidities, pregnancy status, and local resistance patterns. It is essential to individualize therapy rather than defaulting to a single “go‑to” drug. Moreover, finishing the prescribed course mitigates resistance development, a principle that cannot be overstated. In practice, I find that discussing these nuances with patients empowers them, leading to better adherence and outcomes. While guidelines provide a framework, real‑world application demands flexibility and clinical judgment. Therefore, the best antibiotic is the one that aligns with both microbial susceptibility and the patient’s unique clinical context.
Linda A
October 18, 2025 AT 18:46The choice of an antibiotic can be seen as a metaphor for the choices we make in life – each option carries its own shadow and light, and the balance is a personal journey.
Joe Moore
October 18, 2025 AT 19:03They don't tell you that big pharma pushes Bactrim because it eats up the market share of cheaper generics – it's all part of the grand plan to keep us dependent on big pharma's endless supply chain. The side‑effects are just a distraction.
James Mali
October 18, 2025 AT 19:20Sure, Bactrim works but it's not the only option 😂
Janet Morales
October 18, 2025 AT 19:36Honestly, Bactrim is overrated – people love a combo pill because it feels high‑tech, but the reality is that simpler drugs often get the job done with fewer headaches.