When doctors talk about managing inflammatory bowel disease or rheumatoid arthritis, Azulfidine is the brand name you’ll often hear. It contains Sulfasalazine, a drug that has been around for decades, but many patients wonder whether newer options might work better for them. This article breaks down how Azulfidine stacks up against the most common alternatives, so you can see the trade‑offs in efficacy, safety, and cost without having to hunt through multiple sources.
Key Takeaways
- Azulfidine works by releasing an anti‑inflammatory compound directly in the gut, making it a solid first‑line choice for mild‑to‑moderate ulcerative colitis.
- Mesalamine (5‑ASA) offers similar gut‑targeted action with fewer systemic side effects, but may be pricier in some markets.
- Corticosteroids provide rapid symptom relief but are unsuitable for long‑term use because of bone‑loss, diabetes risk, and weight gain.
- Biologic therapies such as infliximab or adalimumab are the most potent options for severe disease but require injections and carry infection risks.
- Cost, insurance coverage, and personal health history often decide which drug is best for an individual.
What Is Azulfidine (Sulfasalazine)?
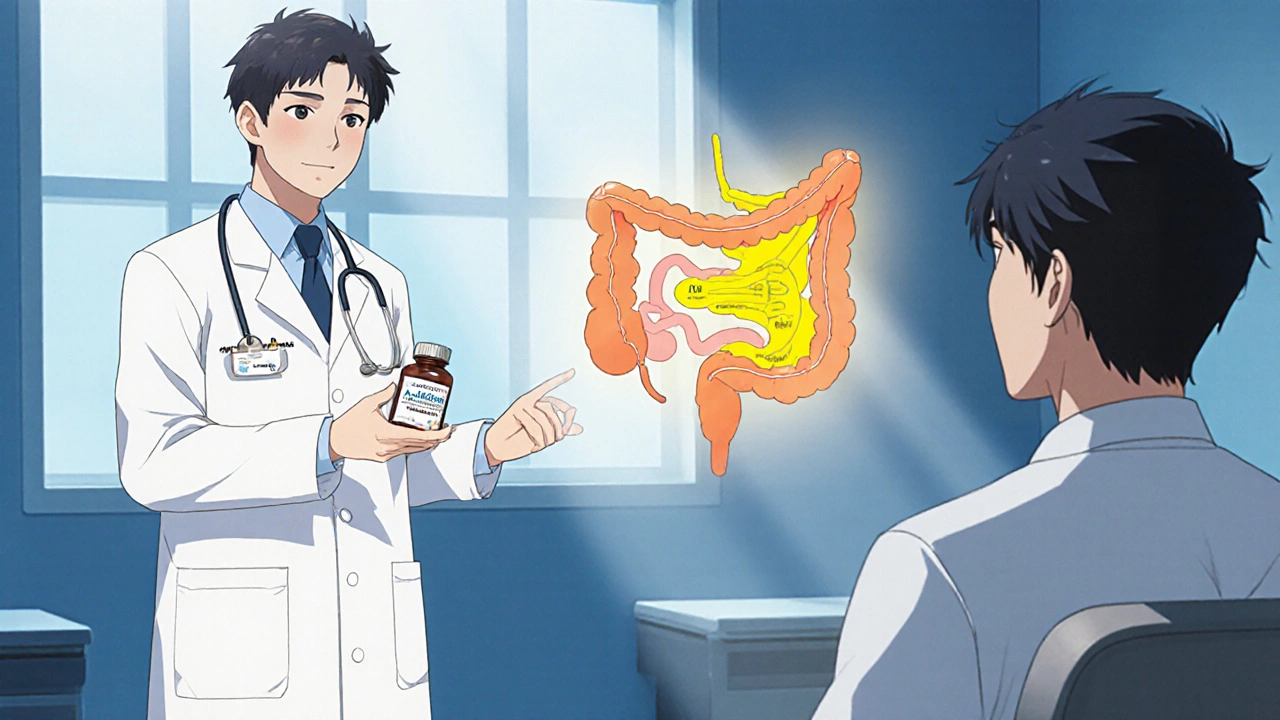
Azulfidine, marketed under the generic name Sulfasalazine, is a sulfonamide antibiotic linked to a 5‑aminosalicylic acid (5‑ASA) molecule. In the colon, bacterial enzymes split the compound, releasing 5‑ASA, which dampens inflammation, and sulfapyridine, which is largely excreted.
It was first approved in the 1950s and remains a staple for both ulcerative colitis (UC) and rheumatoid arthritis (RA). Because it works both locally (in the gut) and systemically, doctors sometimes prescribe it for patients who have joint pain as well as bowel symptoms.
How Sulfasalazine Works
The drug’s dual‑action mechanism gives it a unique profile. In the colon, bacterial azoreductases cleave the sulfasalazine molecule, delivering 5‑ASA right where inflammation occurs. This targeted release reduces the dose needed to achieve symptom control, which can lower the chance of systemic toxicity.
Meanwhile, the sulfapyridine portion is absorbed into the bloodstream and may contribute modestly to the drug’s immunomodulatory effect, which is why it also helps with RA. However, this part is also responsible for some of the classic side effects, such as nausea, rash, and reversible oligospermia.
Alternatives to Azulfidine
When choosing a therapy, doctors weigh disease severity, patient age, comorbidities, and cost. Below are the most frequent alternatives you’ll encounter.
Mesalamine (5‑ASA) Preparations
Products like Asacol, Pentasa, and Lialda deliver 5‑ASA directly to the colon without the sulfapyridine component. This means fewer systemic side effects, especially for patients who are sensitive to sulfonamides. Mesalamine is often prescribed when azathioprine or biologics feel too aggressive for mild disease.
Corticosteroids
Prednisone and budesonide provide rapid inflammation control by broadly suppressing the immune response. They are typically used for short‑term flare management because long‑term exposure leads to bone loss, elevated blood sugar, and adrenal suppression.
Immunomodulators
Drugs such as methotrexate and azathioprine work deeper in the immune cascade and are useful for patients who need steroid‑sparing maintenance therapy. They require regular blood monitoring for liver toxicity and bone‑marrow suppression.
Biologic Therapies
Monoclonal antibodies like infliximab (Remicade), adalimumab (Humira), and vedolizumab (Entyvio) target specific inflammatory pathways (TNF‑α or integrins). They are the most potent options for moderate‑to‑severe UC or RA and are usually administered via infusion or injection.
Side‑by‑Side Comparison
| Drug | Mechanism | Typical Use | Common Side Effects | Cost (USD/month) |
|---|---|---|---|---|
| Azulfidine (Sulfasalazine) | Gut‑released 5‑ASA + sulfapyridine | UC mild‑moderate, RA | Nausea, rash, oligospermia | ~$15-$30 |
| Mesalamine (e.g., Asacol) | Direct 5‑ASA delivery | UC mild‑moderate | Headache, nausea, renal issues | ~$70-$150 |
| Prednisone (systemic steroid) | Broad immune suppression | Flare control (short‑term) | Weight gain, mood swings, osteoporosis | ~$5-$10 |
| Infliximab (biologic) | Anti‑TNF‑α antibody | Moderate‑severe UC, RA | Infusion reactions, infection risk | ~$1,200-$1,500 |
Choosing the Right Therapy
There’s no one‑size‑fits‑all answer, but you can narrow the field by asking four practical questions.
- Disease severity: Mild UC often responds to Azulfidine or mesalamine, while moderate‑to‑severe cases may need biologics.
- Tolerance to sulfonamides: Some patients develop allergic reactions to the sulfapyridine part of sulfasalazine. If that’s a concern, mesalamine is a safer bet.
- Need for rapid relief: Corticosteroids act fastest but are limited to short bursts.
- Financial considerations: Generic Azulfidine is cheap, whereas biologics can be a financial burden without insurance support.
Discuss these points with your gastroenterologist or rheumatologist. They’ll factor in blood test results, previous medication history, and personal lifestyle to land on the most suitable regimen.
Monitoring and Safety
Regardless of the drug you end up on, regular monitoring is essential.
- Blood counts: Sulfasalazine can cause leukopenia, so a CBC every 2-3 months is typical.
- Liver function: Both sulfasalazine and methotrexate affect liver enzymes; check ALT/AST regularly.
- Kidney function: Mesalamine can impair renal clearance; a yearly creatinine test is recommended.
- Infection screening: Before starting biologics, patients are screened for TB and hepatitis B.
Cost and Access Overview
Cost is a decisive factor for many patients.
Azulfidine’s generic status keeps the price low, and most insurance plans cover it with a modest co‑pay. Mesalamine’s price varies widely depending on brand and insurance tier; some plans require prior authorization. Steroids are cheap but may increase long‑term health expenses due to side‑effect management. Biologics are expensive upfront, but many insurers have patient‑assistance programs that can offset a majority of the cost.
When budgeting, also factor in ancillary costs such as infusion center fees for biologics, or the need for regular lab work when using immunomodulators.
Bottom Line
Azulfidine remains a solid, cost‑effective option for patients with mild‑to‑moderate ulcerative colitis or those who also need joint relief. Mesalamine offers a cleaner side‑effect profile at a higher price, steroids provide quick flare control but aren’t suitable for maintenance, and biologics deliver the most powerful disease‑modifying effect at a premium cost and higher infection risk.
Ultimately, the “best” drug is the one that aligns with your disease activity, personal tolerance, lifestyle, and budget. A frank conversation with your healthcare provider, armed with the facts above, will help you land on the right choice.
Frequently Asked Questions
Can I take Azulfidine if I’m allergic to sulfa drugs?
No. Sulfasalazine contains a sulfonamide component, so anyone with a documented sulfa allergy should avoid Azulfidine and opt for a sulfa‑free 5‑ASA like mesalamine.
How long does it take for Azulfidine to start working?
Most patients notice symptom improvement within 2-4 weeks, but full remission can take up to 12 weeks of consistent dosing.
Is it safe to use Azulfidine during pregnancy?
Studies classify sulfasalazine as Category B, meaning animal studies show no risk but human data are limited. Discuss risks and benefits with your obstetrician before starting.
What should I do if I develop a rash while on Azulfidine?
Stop the medication immediately and contact your doctor. A rash can signal a sulfa allergy, and you’ll likely be switched to a non‑sulfa alternative.
Are there natural alternatives that work as well as Azulfidine?
Some patients try probiotics, omega‑3 fatty acids, or curcumin, but evidence shows they are adjuncts rather than replacements for prescription therapy.


10 Comments
Emma Parker
October 22, 2025 AT 20:13Hey! Just a quick heads up – sulfasalazine (Azulfidine) can sometimes give you a weird rash or nausea, so dont brush it off, especially if you’ve got a sulfa allergy. It’s cheap and effective, but keep an eye on any skin changes, ok?
Joe Waldron
October 22, 2025 AT 20:15For anyone considering Azulfidine; remember that its dual mechanism-local 5‑ASA release plus systemic sulfapyridine-offers both gut‑targeted and systemic effects; however, the sulfapyridine moiety is also responsible for side‑effects such as oligospermia, rash, and gastrointestinal upset; regular CBC and liver function monitoring is advisable; dosage adjustments may be needed based on tolerance and disease severity.
Joanne Ponnappa
October 22, 2025 AT 20:16Azulfidine is a solid starter for mild ulcerative colitis 😊. It’s cheap, but if you’re sensitive to sulfa, mesalamine might be a better fit 👍. Always chat with your doc about side‑effects!
Michael Vandiver
October 22, 2025 AT 20:18Azulfidine cheap, works fine! 😊👍
Emily Collins
October 22, 2025 AT 20:20When the gut is on fire, some of us feel like we’re walking through a storm of pain; Azulfidine can be that fragile lifeline, a quiet hero amidst the raging inflammation; yet the sulfapyridine shadow looms, whispering warnings of rash and even impact on fertility; the drama of choosing between relief and risk is real, and every patient must weigh the scales with trembling hands.
Harini Prakash
October 22, 2025 AT 20:21Hey, I hear you – the balance can feel overwhelming, but remember there are ways to mitigate those risks. Monitoring labs regularly, staying hydrated, and discussing any side‑effects early with your doctor can turn that storm into a manageable drizzle. You’re not alone in this journey 😊.
Suryadevan Vasu
October 22, 2025 AT 20:23Azulfidine’s cost‑effectiveness makes it a viable first‑line agent, yet its sulfonamide component necessitates vigilance for hypersensitivity reactions; periodic hematologic assessments are prudent.
Sajeev Menon
October 22, 2025 AT 20:25Totally agree with you, Harini! Keeping those lab checks on schedule can really cut down on surprise side efefcts. And dont forget to ask your doctor about folic acid supplemant if you’re on any other meds.
Wade Grindle
October 22, 2025 AT 20:26Azulfidine works well for many, but if you’re looking for a sulfa‑free option, mesalamine is worth a look.
Sameer Khan
October 22, 2025 AT 20:28Azulfidine (sulfasalazine) remains a cornerstone therapy for mild to moderate ulcerative colitis due to its bifunctional pharmacodynamics, wherein colonic bacterial azo‑reductases cleave the prodrug to liberate 5‑aminosalicylic acid at the site of inflammation while concurrently delivering sulfapyridine systemically. The resultant localized anti‑inflammatory effect mitigates mucosal edema and ulceration, thereby promoting mucosal healing in a proportion of patients comparable to mesalamine derivatives. Nevertheless, the sulfapyridine moiety introduces a distinct adverse event profile, encompassing hypersensitivity reactions, hepatotoxicity, and reversible oligospermia, which necessitates vigilant pharmacovigilance. Clinicians must therefore integrate routine laboratory monitoring, including complete blood counts and liver function tests, at intervals of three months during the induction phase, transitioning to semi‑annual assessments upon disease stabilization. Cost considerations further reinforce the utility of Azulfidine, as its generic formulation yields a monthly expense markedly inferior to that of biologic agents, rendering it accessible across diverse socioeconomic strata. For patients with documented sulfonamide allergy, the risk–benefit calculus shifts unfavorably, prompting selection of sulfa‑free 5‑ASA formulations such as mesalamine, balsalazide, or olsalazine. Moreover, pharmacogenomic data suggest that polymorphisms in N‑acetyltransferase enzymes may modulate sulfapyridine metabolism, influencing both efficacy and toxicity, although routine genotyping remains investigational. In the context of combination therapy, Azulfidine can synergize with immunomodulators like azathioprine, potentially permitting dose reduction of either agent and attenuating steroid dependence. However, the additive immunosuppressive burden mandates comprehensive infectious disease screening, particularly for latent tuberculosis and hepatitis B, prior to initiation. Therapeutic drug monitoring is not routinely performed for sulfasalazine, yet emerging evidence indicates that serum sulfapyridine concentrations correlate with adverse event incidence, suggesting a future role for individualized dosing. Patient adherence is facilitated by the drug’s twice‑daily dosing schedule, though gastrointestinal intolerance may compel formulation adjustments, such as delayed‑release tablets or adjunctive anti‑emetics. Ultimately, the decision matrix for Azulfidine encompasses disease severity, comorbidities, allergy status, economic factors, and patient preference, underscoring the necessity of shared decision‑making in contemporary IBD management. As novel small‑molecule inhibitors and biosimilar biologics expand the therapeutic armamentarium, Azulfidine retains relevance as a cost‑effective, well‑characterized option for appropriate candidates. Continued comparative effectiveness research will elucidate its position relative to emerging agents, ensuring optimized patient outcomes.