When your knees ache every time you stand up, or your hips feel stiff after sitting too long, it’s easy to think rest is the answer. But the truth is, physical therapy might be the most powerful tool you’re not using. For joint disorders like osteoarthritis, rheumatoid arthritis, or even chronic hip pain, movement isn’t the enemy-it’s the medicine. Decades of research now prove that targeted range of motion and strengthening exercises don’t just ease pain-they slow disease progression, delay surgery, and restore real function.
Why Movement Beats Medication for Joint Pain
For years, people with joint disorders were told to pop painkillers and avoid activity. That’s changing fast. The American College of Rheumatology’s 2021 guidelines flipped the script: exercise is now classified as disease-modifying therapy, not just symptom relief. Studies show people who stick with physical therapy have 23% slower joint damage on X-rays compared to those who don’t. That’s not a small benefit-it’s life-altering. A 2023 study in Arthritis & Rheumatology found that for mild-to-moderate hip osteoarthritis, physical therapy delivered the same functional results as total hip replacement-without the surgery. And the cost difference? Medicare data shows patients who do physical therapy before joint replacement cut their total episode costs by 22%. That’s thousands saved, and fewer risks from anesthesia and recovery. The numbers don’t lie. A 2023 review of 127 clinical trials found that structured physical therapy programs reduce pain by 37.6% on average and improve daily function by nearly 30%. Compare that to NSAIDs, which only mask pain without fixing the underlying weakness. And here’s the kicker: physical therapy saves the healthcare system $1,200 to $2,500 per patient each year by reducing doctor visits, imaging, and unnecessary surgeries.Range of Motion: How Much Is Enough?
Range of motion (ROM) isn’t just about bending and stretching. It’s about retraining your nervous system to move without fear. When joints hurt, your body learns to protect them by limiting movement. That leads to stiffness, muscle wasting, and more pain-a vicious cycle. For knee osteoarthritis, the gold standard is terminal knee extension: slowly straightening the knee from a slightly bent position. The 2020 Dutch guidelines recommend 3 sets of 10-15 reps, five days a week, using resistance that feels like 60-70% of your max effort. Pain during exercise should stay under 3 out of 10. If it hits 4 or higher, you’re pushing too hard. For hips, gentle pendulum swings and seated hip marches are often the starting point. Water-based therapy works wonders here-warm water (91-97°F) reduces joint load while allowing freer movement. The American Physical Therapy Association recommends 30-45 minutes, three times a week. Many patients report their first real breakthrough isn’t walking farther-it’s putting on socks without help.Strengthening: The Real Game-Changer
Strengthening is where physical therapy becomes transformative. Weak muscles around a joint mean more stress on the cartilage. Tightening those muscles is like adding shock absorbers to your body. For knee OA, exercises like straight leg raises and step-ups with light ankle weights (2.5 kg) are proven. A 2023 CreakyJoints thread with 112 participants found that terminal knee extension with ankle weights was the single most effective exercise for rising from chairs-a daily task many struggle with. Hip OA requires focused abductor work: side-lying leg lifts, clamshells, or resistance band walks. The 2025 JOSPT guideline recommends 3 sets of 15 reps at 2.5-5.0 kg resistance, three times a week. Progression is slow: increase resistance by only 0.5-1.0 kg per week. Too much too soon causes flare-ups. For rheumatoid arthritis, the American College of Rheumatology advises resistance training at 40-60% of your one-rep max, twice a week. That’s not heavy lifting-it’s controlled, consistent effort. One patient, 68, with RA, told her therapist, “I didn’t think I’d ever carry groceries again. Now I do it without thinking.”
What Doesn’t Work-and Why
Not all exercise helps. Generic routines-like doing 50 squats because “it’s good for knees”-often backfire. A 2022 study found that generic exercise prescriptions only work for 12-15% of patients. But when a physical therapist personalizes the program based on your pain levels, joint damage, and strength deficits, success jumps to 65-70%. Physical therapy also has limits. If X-rays show more than 50% joint space narrowing, exercise alone won’t rebuild cartilage. That doesn’t mean it’s useless-it still improves muscle control, reduces pain, and prepares you for surgery if needed. In fact, prehabilitation (pre-surgery PT) cuts post-op complications by 31% and shortens hospital stays by nearly two days, according to Cleveland Clinic data. Another myth: rest equals healing. Inactivity leads to faster muscle loss. One study found that just two weeks of bed rest in older adults with knee OA resulted in a 25% drop in quadriceps strength. That’s why even on bad days, gentle movement matters.Real People, Real Results
On Healthgrades, physical therapy for joint disorders holds a 4.2 out of 5 rating from over 14,800 reviews. The most common success stories? “I can climb stairs again.” “I stopped using my cane.” “I played with my grandkids without pain.” But it’s not all smooth sailing. Reddit threads in r/Physical_Therapy show that 41% of patients experience increased pain in the first two weeks. That’s normal-it’s your body adapting. But if pain lasts longer than 48 hours after a session, talk to your therapist. You might need to adjust the load or technique. Insurance is another hurdle. 58% of negative reviews on Yelp mention session limits. Medicare covers up to 30 sessions per year for joint disorders, but many private insurers cap it at 10-20. That’s often not enough. The good news? Starting in 2026, Medicare will expand coverage for maintenance therapy for chronic joint conditions, recognizing that ongoing care is part of managing the disease.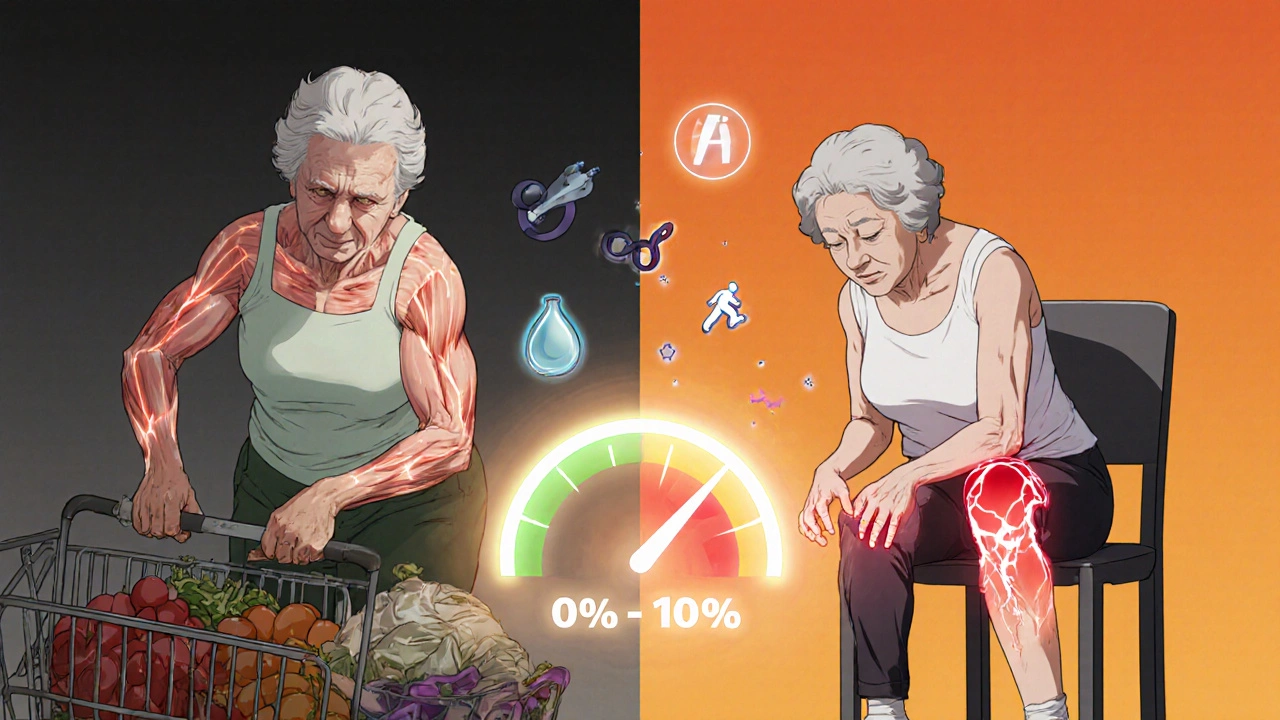
How to Get Started
You don’t need a referral in most states, but your doctor’s support helps with insurance. Look for a physical therapist with orthopedic certification (OCS) or specialized training in joint disorders. They should:- Assess your joint mobility, muscle strength, and pain triggers
- Use validated tools like the HOOS (for hips) or KOOS (for knees) to track progress
- Set clear goals: “Walk 10 minutes without pain” or “Get out of bed without using hands”
- Adjust your program weekly based on your feedback
The Future Is Personalized
The field is evolving fast. The 2025 JOSPT hip osteoarthritis guideline now uses machine learning to predict who will respond best to which exercises-based on your HOOS score, BMI, and X-ray results. Accuracy? 83%. Telehealth is booming too. New billing codes as of January 2025 let therapists bill for remote sessions using wearable sensors that track movement quality. If you live in a rural area with no local clinic, you can now get real-time feedback from your therapist via video and motion sensors. Emerging tech like neuromuscular electrical stimulation (NMES) is showing promise. A 2024 University of Pittsburgh study found that adding NMES to exercise boosted strength gains by 41% in knee OA patients at 24 weeks.Bottom Line: Move Smart, Not Hard
Physical therapy for joint disorders isn’t about pushing through pain. It’s about moving with precision, consistency, and patience. You don’t need fancy equipment. You don’t need to be an athlete. You just need to show up-and let your body rebuild itself, one controlled movement at a time. The data is clear: if you have joint pain, physical therapy isn’t a last resort. It’s the first, best, and most cost-effective step you can take.How long does physical therapy take to work for joint pain?
Most people notice improved mobility and reduced pain within 4 to 6 weeks of consistent therapy. Significant functional gains-like climbing stairs or standing from a chair without help-typically occur by week 8. Full results, including strength gains and long-term pain reduction, often take 12 to 16 weeks. Adherence is key: patients who complete 70% or more of their prescribed exercises see the best outcomes.
Can physical therapy replace surgery for severe joint damage?
For mild-to-moderate joint damage, physical therapy can delay or even eliminate the need for surgery. Studies show it provides equivalent functional results to hip replacement in patients with early osteoarthritis. But if X-rays show more than 50% joint space narrowing, exercise alone won’t restore cartilage. In those cases, PT still helps by improving muscle control, reducing pain, and preparing the body for surgery-leading to faster recovery and fewer complications.
Is it normal to feel more pain after a physical therapy session?
Mild discomfort during or right after a session is normal, especially in the first two weeks. This is your muscles and joints adapting. Pain should stay below 3 out of 10 during exercise and resolve within 48 hours. If pain worsens, lasts longer than two days, or feels sharp or shooting, your therapist needs to adjust your program. Pushing through severe pain can cause injury and set back progress.
What if I can’t afford or access physical therapy?
Cost and access are real barriers. Rural patients are 2.4 times more likely to quit therapy due to transportation issues. If you can’t get in-person care, ask your provider about telehealth options-new billing codes now cover remote sessions with motion-tracking wearables. Many clinics offer sliding scale fees. You can also follow evidence-based home programs from reputable sources like the Arthritis Foundation or the American Physical Therapy Association. Consistency matters more than equipment: bodyweight squats, heel slides, and seated leg lifts can be done daily with no cost.
How often should I do strengthening exercises for joint disorders?
For most joint disorders, 2 to 3 days per week is ideal. The American College of Rheumatology recommends resistance training twice weekly at 40-60% of your one-rep max. For osteoarthritis, the 2025 JOSPT guidelines suggest 3 sets of 15 reps at moderate resistance (2.5-5.0 kg) three times a week. Rest at least one day between sessions to allow muscles to recover. More isn’t better-overtraining increases flare-up risk. Progress slowly: increase resistance by only 0.5-1.0 kg per week.
What’s the difference between range of motion and strengthening exercises?
Range of motion (ROM) exercises focus on moving your joint through its full, pain-free movement-like gently bending and straightening your knee. They reduce stiffness and improve flexibility. Strengthening exercises build muscle around the joint to support and protect it-like lifting your leg sideways to target hip abductors. ROM comes first, especially in early stages. Once pain decreases, strengthening is added to prevent future damage. Both are essential and work together.



9 Comments
king tekken 6
November 29, 2025 AT 00:00man i used to think rest was the answer too until my knee started acting like a rusty hinge at 3am
physical therapy felt like torture at first but now i can climb stairs without crying
turns out your body ain't broken, it's just lazy and scared
also i stopped taking ibuprofen like a drug addict and my stomach stopped hating me
who knew movement was the medicine and not the problem?
DIVYA YADAV
November 29, 2025 AT 10:40you think this is about health? no this is big pharma's plan to sell you gadgets and make therapists rich
why don't you ask why the government pushes PT but hides the truth about glyphosate destroying our joints?
indian farmers used to walk miles and never needed PT until the west sold them processed food and fake medicine
they don't want you strong-they want you dependent on clinics and insurance
the real cure? return to traditional diets and natural movement-no machines, no bills, no lies
Kim Clapper
November 29, 2025 AT 11:48I find it deeply concerning that this article presents physical therapy as a benign, universally applicable solution without acknowledging the systemic erosion of patient autonomy in modern healthcare.
Who decides what 'moderate resistance' means? Who funds the studies cited? Are the therapists certified? Are they incentivized to push patients beyond safe limits?
And yet, we are told to trust the data-while the same institutions that endorse this protocol also approve pharmaceuticals with lethal side effects.
There is a quiet coercion here, masked as empowerment.
It is not movement that heals-it is compliance.
And compliance, my dear reader, is the most profitable commodity in medicine today.
Bruce Hennen
December 1, 2025 AT 05:26Wrong. The 2023 CreakyJoints thread cited has a sample size of 112, which is not statistically significant for a population of 30 million Americans with knee OA.
Also, the 22% cost reduction claim is from Medicare data, which excludes private insurance and out-of-pocket expenses-misleading framing.
And the 37.6% pain reduction? That's a mean. Median might be 21%. You're cherry-picking the best-case scenario.
Also, 'terminal knee extension' isn't a term used in clinical guidelines-it's a buzzword.
Real science requires replication, not blog posts dressed as peer-reviewed.
Jake Ruhl
December 2, 2025 AT 16:14ok so here's the truth no one tells you
physical therapy is just a fancy word for 'do stuff your grandma did in 1978'
they make you do leg lifts and pretend it's science
and yeah it works but not because of some fancy study
it works because you stop sitting on your butt all day
also i tried it after my knee surgery and honestly the first week i wanted to quit
but then one day i bent over to tie my shoe and didn't scream
and that was it
i didn't need a degree to know that was magic
so stop overcomplicating it
just move
even if it hurts
even if it's slow
even if your therapist says 'you're doing great'
you're not
but you're trying
and that's enough
Chuckie Parker
December 2, 2025 AT 16:51PT is a scam if you live in a rural town and have to drive 90 minutes to get there
insurance only covers 10 visits
you get 3 weeks of hope then they drop you
and then you're back to painkillers and silence
they sell you a dream then take it away because you're not worth the cost
they don't care if you walk again
they care if your claim is closed
the system is rigged
and the data? Just marketing
don't believe the hype
you're on your own
Aarti Ray
December 4, 2025 AT 03:48in india we dont have access to PT like this but my aunt did heel slides every morning on the floor with a towel
no machines no cost
just patience
she couldnt bend to pick up her sari for years
now she dances at weddings again
its not about the tech
its about showing up
even if its just 5 minutes
even if its messy
even if your neighbor laughs
you keep going
because your body remembers how to move
even when your mind forgets
Alexander Rolsen
December 5, 2025 AT 00:33Let me be clear: the entire physical therapy industry is a profit-driven illusion.
They sell you hope wrapped in a clipboard.
They tell you ‘consistency matters’-but only if you can afford 40 sessions.
They cite studies funded by equipment manufacturers.
They ignore the fact that 41% of patients report increased pain-yet call it ‘normal adaptation.’
It’s not adaptation-it’s exploitation.
You’re not healing-you’re being monetized.
And the worst part? You believe them.
Because you’re desperate.
And they know it.
Leah Doyle
December 6, 2025 AT 03:56My grandma started PT after her hip replacement and cried the first week... then she laughed because she could hug her grandkids without wincing 😭
It wasn't magic, it was just... showing up.
Even on days when she wanted to quit, she did 3 reps.
And now? She walks to the mailbox every morning.
Not because of studies or stats.
Because someone believed she could.
And she believed herself.
Thank you for writing this. It made me cry happy tears.
❤️