Medication Dizziness Risk Checker
Check how your current medications may affect your dizziness risk. This tool uses data from the latest clinical studies to estimate your risk level.
Based on the medications you've selected, your dizziness risk level is shown above.
Commonly prescribed for seizures, this class is among the highest risk for dizziness. May cause balance problems and vertigo.
Often used for depression and chronic pain. Can cause dizziness, especially when standing up quickly.
Commonly prescribed for depression and anxiety. Dizziness often improves after initial adjustment period.
Helps manage fluid retention but can cause orthostatic hypotension. Be careful when standing up.
Used for blood pressure, heart conditions, and migraines. Can cause dizziness and fatigue.
Common blood pressure medication that may cause dizziness due to blood pressure drop.
Potentially dangerous for balance. Can cause permanent inner ear damage. Use with caution.
Commonly used for acid reflux. Dizziness is less common but still possible with long-term use.
Feeling dizzy or lightheaded after taking a new pill? You’re not alone. About dizziness affects 1 in 5 adults every year, and nearly a quarter of those cases are directly linked to medications. It’s not just a nuisance-it can lead to falls, hospital visits, and even long-term balance problems, especially for older adults. The good news? Most cases are manageable once you know what’s causing them.
How Medications Make You Feel Dizzy
Dizziness isn’t one thing. It can feel like the room is spinning (vertigo), like you’re about to pass out (lightheadedness), or just unsteady on your feet. Medications trigger these feelings in three main ways: by messing with your inner ear, lowering your blood pressure too much, or changing brain chemicals.Your inner ear holds tiny hair cells that help your brain understand where your body is in space. Some drugs, like the antibiotic gentamicin, can kill those cells. Studies show 17% to 40% of people on long-term gentamicin develop permanent damage. Chemotherapy drugs like cisplatin are even worse-up to 65% of patients lose vestibular function after standard treatment. That’s not rare. It’s expected.
Then there’s blood pressure. Many people take meds to lower it, but sometimes they drop too fast. Standing up too quickly after taking an ACE inhibitor like lisinopril or a diuretic like furosemide can cause your blood pressure to plummet. That’s called orthostatic hypotension. It’s why you feel faint when you stand. About 14% of lisinopril users and 22% of furosemide users report this. Beta-blockers like propranolol cause dizziness in nearly 20% of users.
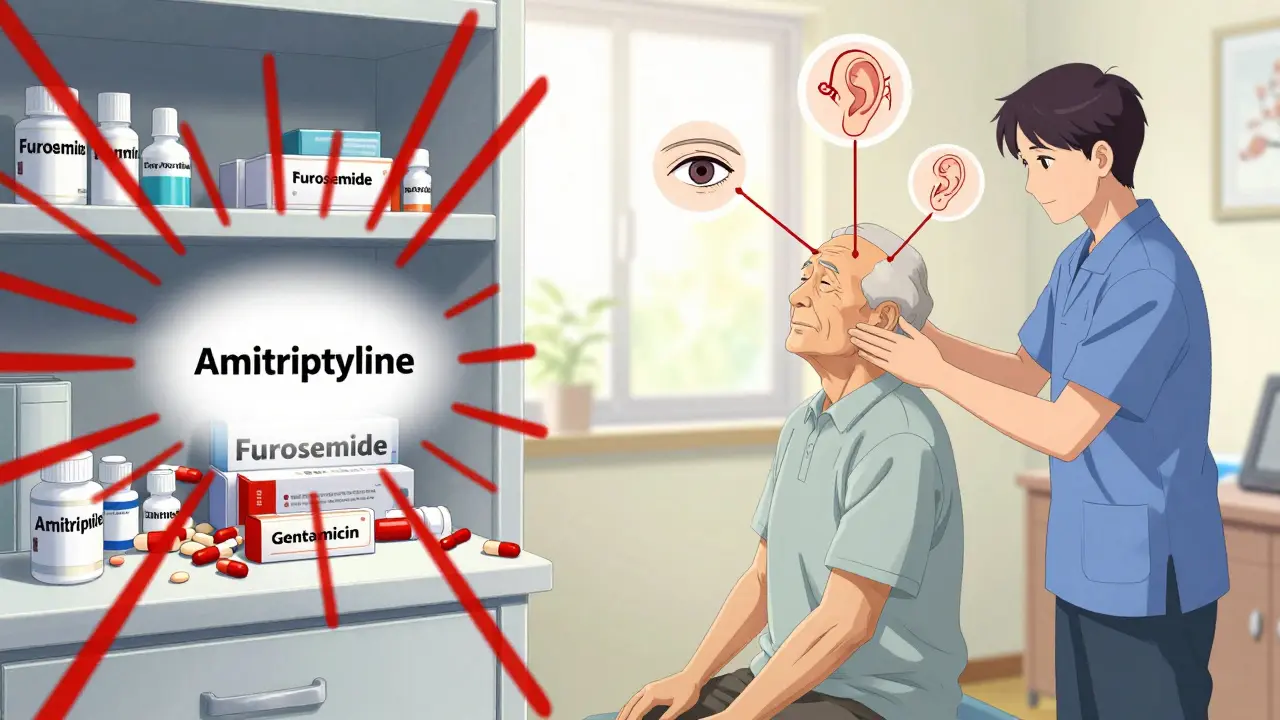
And then there’s your brain. Antidepressants-especially SSRIs like fluoxetine and tricyclics like amitriptyline-alter serotonin and norepinephrine levels. That can throw off signals between your eyes, inner ear, and muscles. Up to 28% of people on amitriptyline feel dizzy in the first few weeks. Even common drugs like proton pump inhibitors (omeprazole) can cause it, though less often. Millions take them daily, so even a 5% rate adds up to thousands of cases.
Which Medications Are Most Likely to Cause Dizziness?
Not all drugs are equal when it comes to dizziness. Some are far riskier than others. Here’s what the data shows:| Medication Class | Example Drug | Dizziness Rate |
|---|---|---|
| Antiepileptic | Carbamazepine | 29.7% |
| Antidepressant (Tricyclic) | Amitriptyline | 28.4% |
| Antidepressant (SSRI) | Fluoxetine | 25.3% |
| Diuretic | Furosemide | 22.1% |
| Beta-blocker | Propranolol | 19.7% |
| ACE Inhibitor | Lisinopril | 14.2% |
| Aminoglycoside Antibiotic | Gentamicin | 17-40% |
| Proton Pump Inhibitor | Omeprazole | 5.2% |
What’s surprising? Benzodiazepines (like diazepam) and first-generation antihistamines (like diphenhydramine) aren’t on this list-but they’re just as dangerous for older adults. The American Geriatrics Society lists them as high-risk because they increase fall risk by 40-50%. These drugs slow down your brain’s ability to process balance signals. For someone over 65, that’s a recipe for a broken hip.
Why Older Adults Are at Higher Risk
If you’re over 65, your body handles drugs differently. Your liver and kidneys don’t clear medications as quickly. Your blood pressure control weakens. Your inner ear hair cells naturally decline with age. And if you’re taking five or more medications-a common situation known as polypharmacy-your chance of dizziness jumps by 300%.One study of over 12,000 older adults found that those on five or more drugs were far more likely to report dizziness than those on just one. And it’s not just the drugs themselves-it’s how they interact. A blood pressure pill plus a sleep aid plus an antidepressant? That’s a triple threat. The American Geriatrics Society’s 2023 Beers Criteria warns against 17 specific drugs for seniors because of this exact risk. Many of these are still prescribed regularly, often because doctors don’t realize how dangerous they are for older bodies.
And here’s the kicker: dizziness is often dismissed as “just aging.” But it’s not normal. It’s a warning sign. Falls are the leading cause of injury-related death in seniors. About 35% of people over 65 fall at least once a year-and nearly half of those falls are linked to medications.
What to Do If You’re Feeling Dizzy
Don’t ignore it. Don’t assume it’s just stress or lack of sleep. Start tracking.Keep a simple diary for two weeks. Write down:
- When you took each medication
- When you felt dizzy (time of day, activity)
- How long it lasted
- Any other symptoms (ringing in ears, nausea, blurred vision)
Studies show 68% of medication-related dizziness follows a clear pattern-like happening 30 minutes after taking a pill. That’s a huge clue.
Then talk to your doctor. Don’t stop anything on your own. Stopping seizure meds suddenly can triple your risk of seizures. Stopping beta-blockers cold turkey can trigger a heart attack. Your doctor may use the Naranjo Scale, a tool that rates how likely a drug is to cause the side effect. A score of 9 or higher means it’s almost certainly the drug.
How Doctors Manage It
Good doctors don’t just say, “It’s a side effect-deal with it.” They follow a clear plan:- Confirm the link: A 4- to 6-week trial of stopping or lowering the dose (under supervision) to see if dizziness improves.
- Check fall risk: Using tools like the Hendrich II Fall Risk Model to see how likely you are to fall.
- Switch meds: If possible, pick a similar drug with less dizziness risk. For example, switching from amitriptyline to sertraline can cut dizziness in half.
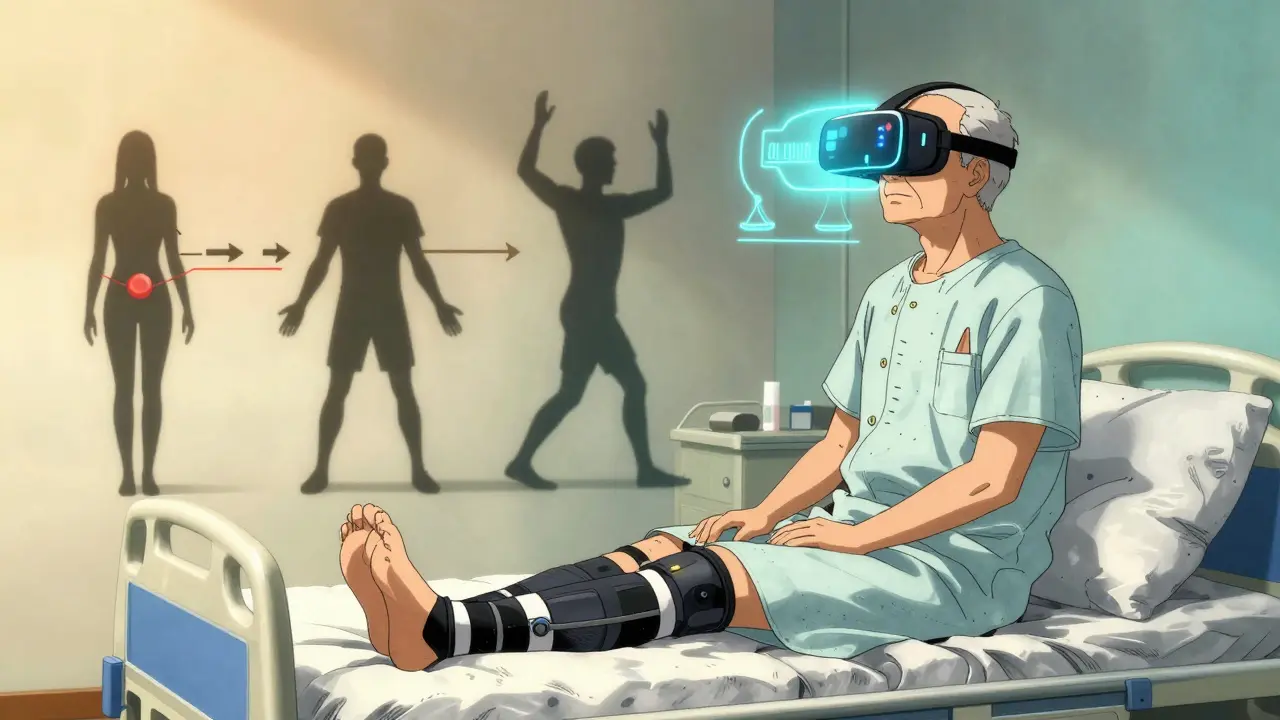
- Use non-drug fixes: Vestibular rehabilitation therapy (VRT) is proven to work. It’s a series of simple exercises-like moving your head slowly while focusing on a fixed point-that retrain your brain to rely on other balance signals. Studies show 70-80% of people see major improvement after 6-8 sessions.
For orthostatic dizziness, simple tricks help: sit on the edge of the bed for a minute before standing, wear compression stockings, and drink more water. One 2022 trial found compression stockings reduced dizziness by 45% in older adults on blood pressure meds.
When to Worry
Most dizziness from meds is temporary. But some signs mean you need urgent care:- Dizziness that comes with chest pain, shortness of breath, or irregular heartbeat
- Sudden hearing loss or ringing in one ear
- Double vision, slurred speech, or weakness on one side
- Dizziness that doesn’t improve after stopping the drug
These could signal something more serious-like a stroke, heart problem, or permanent nerve damage. Don’t wait. Get checked.
What’s Changing in 2026
Medicine is catching up. In 2024, the American Heart Association updated its guidelines to require both dizziness symptoms AND a clear blood pressure drop to diagnose orthostatic hypotension. The International Headache Society now officially recognizes “medication-induced vestibular syndrome” as its own diagnosis.And the future? Personalized medicine. A 2023 study found 17 genetic variants that make some people way more likely to get dizzy from blood pressure meds. Soon, we may test your DNA before prescribing a drug to see if you’re at high risk.
Virtual reality rehab is also gaining ground. One 2023 trial used VR headsets to simulate balance challenges-and 82% of patients improved. It’s not in every clinic yet, but it’s coming fast.
The American Geriatrics Society is updating its Beers Criteria later in 2024, and it may add newer diabetes drugs like SGLT2 inhibitors, which showed nearly 10% dizziness rates in recent data. That’s a red flag for millions of older adults on these drugs.
Bottom Line
Dizziness from medication isn’t something you have to live with. It’s a signal-not a sentence. Track your symptoms. Talk to your doctor. Ask if there’s a safer alternative. And never stop a drug without their guidance.The goal isn’t to avoid all meds-it’s to use the right ones, at the right dose, for your body. Balance matters. So does safety. And you deserve both.
Can dizziness from medication go away on its own?
Yes, in many cases. If the dizziness is caused by starting a new medication, it often improves within a few days to weeks as your body adjusts. But if it persists beyond 4-6 weeks, or gets worse, it’s likely not just an adjustment phase. That’s when you need to talk to your doctor about switching or lowering the dose. Permanent damage from drugs like gentamicin or cisplatin won’t go away, but symptoms can still be managed with therapy.
Are over-the-counter meds safe if they cause dizziness?
Not always. Many OTC drugs like diphenhydramine (Benadryl), motion sickness pills, and even some sleep aids cause dizziness by blocking acetylcholine in the brain. These are especially risky for older adults and can increase fall risk by 40%. Just because they’re sold without a prescription doesn’t mean they’re harmless. Always check labels for dizziness as a side effect, and talk to your pharmacist before mixing them with other meds.
Can I take vitamins or supplements to prevent medication-induced dizziness?
There’s no proven supplement that prevents dizziness caused by drugs. Some people think magnesium or B12 helps, but studies don’t support that for medication-related cases. In fact, some supplements like ginkgo biloba or garlic can interact with blood pressure meds and make dizziness worse. The safest approach is to focus on proven strategies: tracking symptoms, adjusting meds under medical supervision, and doing vestibular rehab if needed.
Is vestibular rehabilitation therapy covered by insurance?
In most cases, yes. In the U.S., Medicare and many private insurers cover vestibular rehabilitation when prescribed by a doctor and delivered by a licensed physical or occupational therapist with vestibular training. In Australia, it’s often covered under Medicare’s Chronic Disease Management plan if your GP refers you. Check with your provider, but don’t assume it’s not covered-this therapy is medically recognized and highly effective.
Should I avoid all medications that list dizziness as a side effect?
No. Many of these drugs are essential-like blood pressure meds for preventing stroke, or antidepressants for severe depression. The goal isn’t to avoid them, but to use them wisely. If you’re at high risk (older, on multiple drugs, or have balance issues), your doctor can choose alternatives with lower dizziness risk. For example, switching from a beta-blocker to a calcium channel blocker might help. Always weigh the benefit against the risk. Sometimes the dizziness is worth it if the drug saves your life.
How long does it take to recover from vestibular damage caused by medication?
If the damage is permanent-like from cisplatin or gentamicin-your inner ear hair cells won’t grow back. But your brain can adapt. Vestibular rehabilitation helps your brain rely on your vision and body sensors instead. Most people regain significant function within 3-6 months of therapy. Full recovery isn’t always possible, but most patients can return to normal daily life with consistent therapy. Early intervention makes a big difference.
Next Steps
If you’re experiencing dizziness and take any medications:- Start a symptom diary today.
- Make a list of every pill, patch, or supplement you take-include doses and times.
- Ask your doctor: “Could any of these be causing my dizziness?”
- Ask if vestibular rehab is an option.
- Never stop a drug without talking to your provider first.
Dizziness isn’t just a side effect. It’s a signal your body is sending. Listen to it. Act on it. Your balance-and your safety-depend on it.



8 Comments
Ryan Riesterer
January 23, 2026 AT 04:25The vestibular toxicity profile of aminoglycosides is well-documented in ototoxicity literature, with gentamicin inducing dose-dependent hair cell apoptosis via mitochondrial ROS generation. The 17–40% incidence aligns with longitudinal cohort data from the Journal of Neuro-Otology. Clinically, this is non-reversible; compensation relies on central vestibular plasticity. Monitoring with vHIT and cVEMP is recommended during prolonged therapy.
Mike P
January 24, 2026 AT 19:02Oh wow, so now we’re blaming doctors for giving people medicine? Get a grip. If you can’t handle a little dizziness, maybe you shouldn’t be on meds at all. My grandpa’s on six drugs and still mows his lawn. You people act like a pill is gonna kill you. Chill the hell out. It’s not 1999 anymore - we’ve got science, not witchcraft.
Sarvesh CK
January 25, 2026 AT 23:34It is profoundly instructive to observe how modern pharmacology, while undeniably efficacious in managing chronic conditions, inadvertently introduces iatrogenic vulnerabilities in the elderly population. The convergence of polypharmacy, age-related physiological decline, and insufficient pharmacokinetic recalibration constitutes a systemic oversight in geriatric care. One cannot help but reflect on the ethical imperative to prioritize functional autonomy over pharmacological convenience. The data presented here underscores not merely a clinical challenge, but a civilizational one - how do we care for those who have cared for us, when our tools, however advanced, remain blunt instruments in the face of biological complexity?
Daphne Mallari - Tolentino
January 27, 2026 AT 16:09It’s remarkable how casually this post dismisses the importance of patient agency. The reliance on anecdotal symptom diaries, while well-intentioned, lacks the rigor of controlled pharmacovigilance protocols. One wonders whether the recommendation to ‘talk to your doctor’ is sufficient when primary care providers are averaging 7 minutes per visit. This is not medicine - it’s triage dressed up as empowerment.
Neil Ellis
January 28, 2026 AT 04:58Man, this post is like a love letter to your body’s warning system. Dizziness? That’s your inner ear screaming, ‘Hey, something’s off!’ And instead of just popping another pill, we’re finally starting to listen. Vestibular rehab? It’s like yoga for your brain - slow, weird, but totally life-changing. I’ve seen people who couldn’t walk straight get back to hiking after 8 sessions. No magic, just science with heart. Don’t ignore the whispers - your balance is your freedom.
Rob Sims
January 29, 2026 AT 11:06Oh great, another ‘meds are evil’ fearmongering article. Let me guess - next you’ll tell us aspirin causes brain rot? People get dizzy on lisinopril? Shocking. Next you’ll say oxygen causes dizziness if you breathe too fast. Wake up. The risk is low, the benefit is high. Stop being hypochondriacs and take your damn pills. Your doctor didn’t become a doctor to babysit your anxiety.
arun mehta
January 30, 2026 AT 20:33Thank you for this deeply thoughtful piece 🙏. As someone from India where polypharmacy is rampant due to over-the-counter access, I’ve seen too many elders suffer silently. The 300% increase in dizziness with 5+ meds? That’s not statistics - that’s my aunt. Vestibular rehab is underused here, but we’re starting pilot programs in Chennai. Small steps. Also, OTC diphenhydramine? It’s sold like candy. We need regulation, not just awareness. 🌏❤️
Lauren Wall
January 31, 2026 AT 16:28My grandma fell last year. Turns out it was the ZzzQuil and the blood pressure pill. She’s off both now. No dizziness. No falls. Simple.