When your kidneys start to fail, they don’t just stop filtering waste. They also stop managing the minerals that keep your bones strong and your heart safe. This is where CKD-MBD - Chronic Kidney Disease-Mineral and Bone Disorder - comes in. It’s not just about weak bones. It’s a silent, systemic breakdown of calcium, phosphorus, parathyroid hormone (PTH), and vitamin D that affects nearly every organ in your body. By Stage 3 of kidney disease, this process is already underway. By dialysis, it’s almost universal.
What Exactly Is CKD-MBD?
CKD-MBD isn’t a single problem. It’s a chain reaction. When kidneys lose function, they can’t remove excess phosphorus from your blood. That buildup triggers your body to make more fibroblast growth factor 23 (FGF23), a hormone that tries to force the kidneys to dump more phosphorus. But damaged kidneys can’t respond. So FGF23 levels spike - sometimes 1000 times higher than normal.
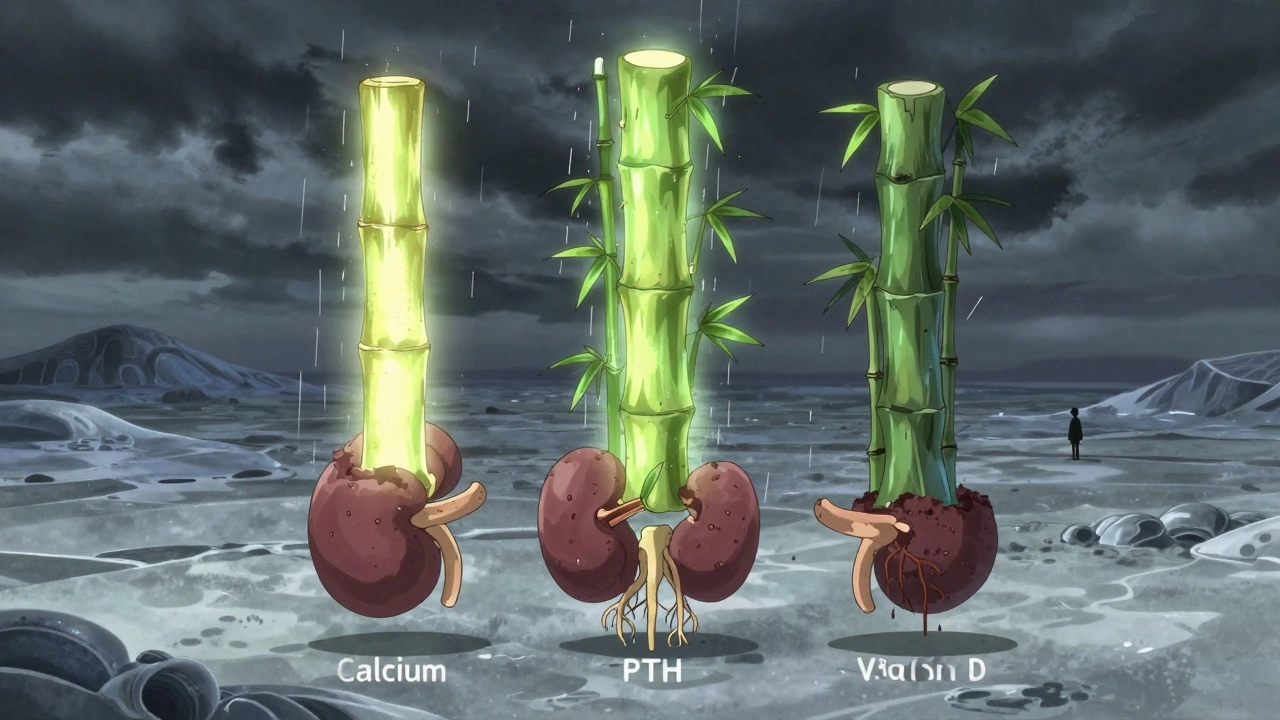
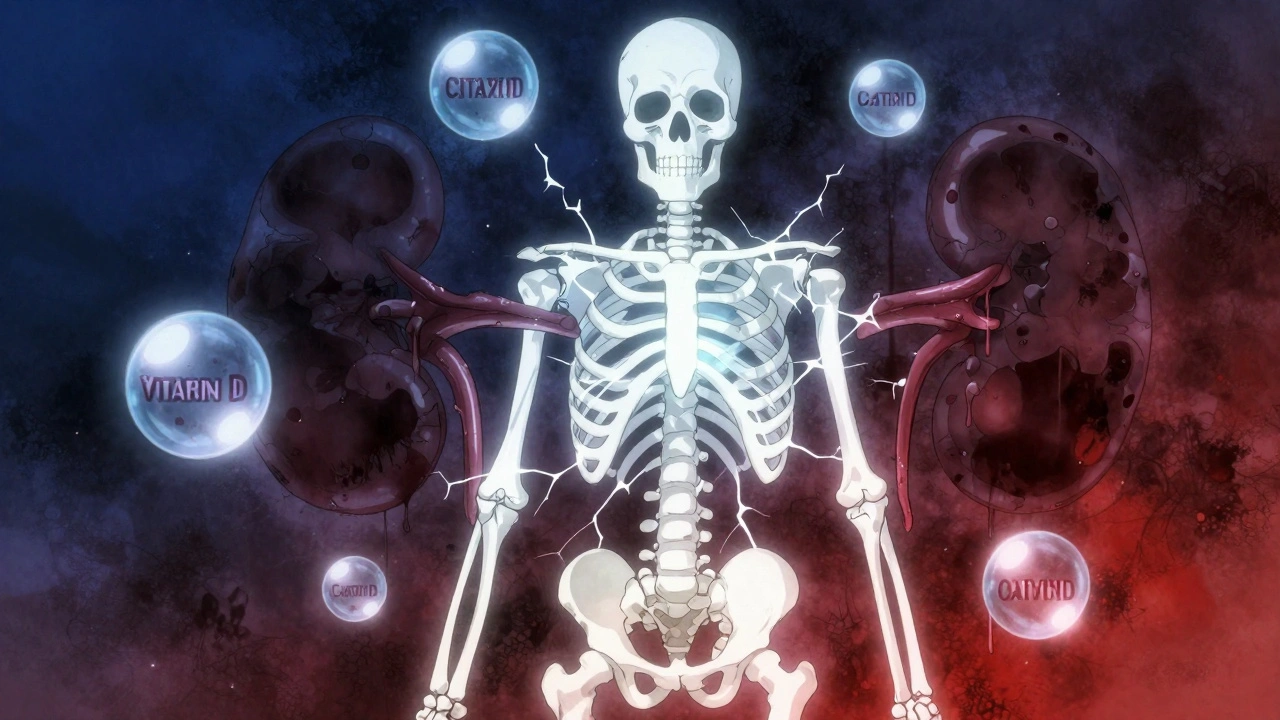
At the same time, your kidneys stop converting vitamin D into its active form, calcitriol. Without enough calcitriol, your gut can’t absorb calcium properly. Your blood calcium drops. Your parathyroid glands, sensing this drop, go into overdrive. They swell up and pump out more PTH to pull calcium out of your bones. This is called secondary hyperparathyroidism.
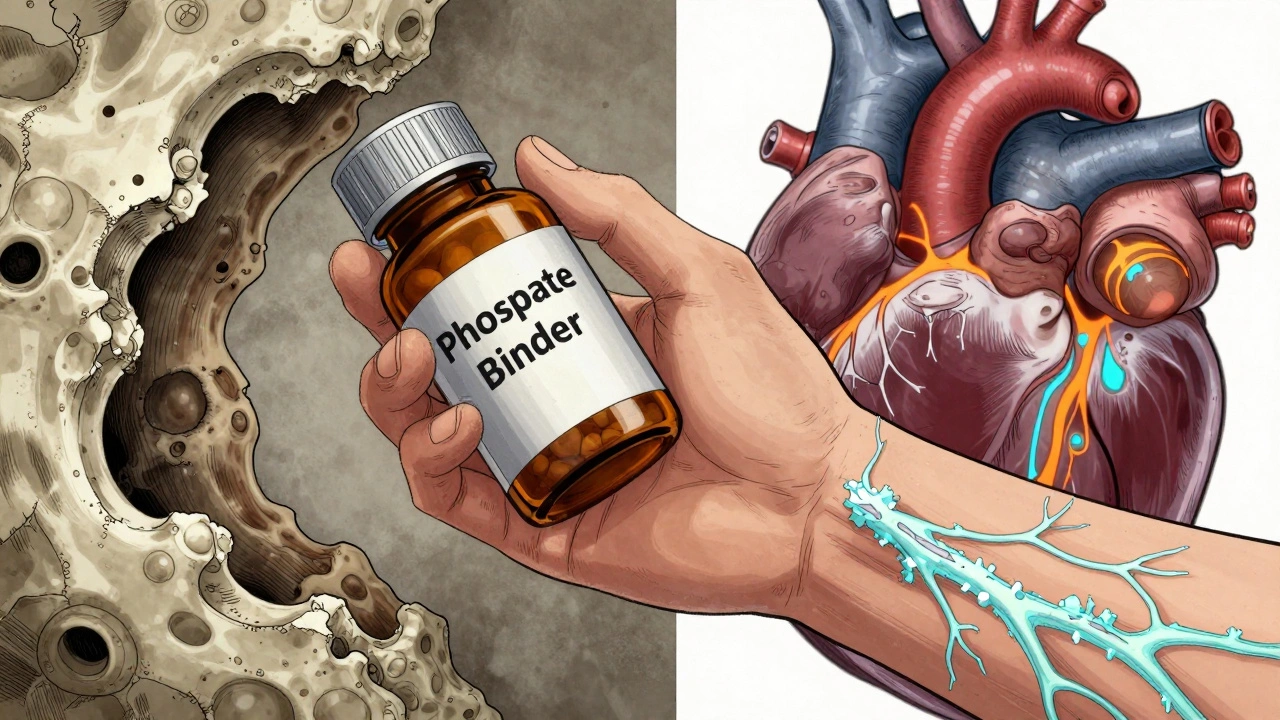
But here’s the twist: even with sky-high PTH levels, your bones stop responding. They become resistant. So instead of getting stronger, they get brittle. Meanwhile, calcium and phosphorus start sticking to your blood vessels, heart valves, and lungs. This isn’t just plaque. It’s actual hardening - like rust inside your arteries. And that’s why people with advanced kidney disease are five times more likely to die from heart problems than from kidney failure itself.
The Three Pillars: Calcium, PTH, and Vitamin D
These three aren’t just numbers on a lab report. They’re the heartbeat of CKD-MBD.
Calcium should stay between 8.4 and 10.2 mg/dL. Too low? Your bones dissolve. Too high? Your arteries calcify. Most people think low calcium is the problem. But in CKD, it’s rarely that simple. Often, calcium is normal - but only because your bones are giving up their stores to keep blood levels stable. That’s why you can’t judge bone health by blood calcium alone.
PTH is the alarm bell. Normal levels are 10-65 pg/mL. In Stage 3 CKD, PTH may already be above 65. By Stage 5D (dialysis), over 80% of patients have PTH levels above 300. But here’s the trap: if PTH drops too low - below 150 - you get something called adynamic bone disease. Your bones stop remodeling. They become stiff, dense, and just as likely to break. That’s why doctors don’t just want to crush PTH. They want to keep it in a narrow window: 2 to 9 times the upper limit of normal. Too high? Bone loss. Too low? Bone death.
Vitamin D is the forgotten player. Over 80% of people with Stage 3-5 CKD are deficient in 25-hydroxyvitamin D. That’s the storage form. Your body needs it to make calcitriol - the active hormone. But your kidneys can’t do that anymore. So giving you more vitamin D isn’t just about fixing a deficiency. It’s about slowing the whole cascade. Studies show that correcting vitamin D levels with cholecalciferol (D3) cuts mortality risk by 15%. Active forms like calcitriol or paricalcitol? They’re reserved for extreme cases - because they can spike calcium and phosphorus dangerously.
Bone and Blood Vessels: The Same Problem
For decades, doctors called this condition “renal osteodystrophy.” That name focused only on the bones. But we now know: the same forces that destroy your skeleton are calcifying your heart.
There are three main bone patterns in CKD-MBD:
- High turnover disease (osteitis fibrosa cystica): Caused by long-term high PTH. Bones are porous, weak, and fracture easily. Seen in 20-30% of dialysis patients.
- Low turnover disease (adynamic bone disease): Bones don’t rebuild. They’re dense but fragile. PTH is low. This is now the most common type - affecting 50-60% of dialysis patients. Often caused by too much calcium-based binder or overuse of active vitamin D.
- Mixed disease: A blend of both. Seen in 10-20% of cases.
And the vascular damage? It’s worse than you think. Coronary artery calcification scores are 3-5 times higher in dialysis patients than in healthy adults. Every year, calcification progresses by 15-20%. That’s not gradual aging. That’s accelerated decay. And every 1 mg/dL rise in serum phosphate? That’s an 18% higher risk of dying.
How Is It Diagnosed?
You won’t feel CKD-MBD until it’s advanced. No pain. No swelling. Just silent damage.
Doctors check:
- Serum phosphate: Target 2.7-4.6 mg/dL for Stage 3-5, 3.5-5.5 for dialysis
- Serum calcium: 8.4-10.2 mg/dL
- Intact PTH: 2-9 times the upper normal limit (varies by lab)
- 25-hydroxyvitamin D: At least 30 ng/mL
Bone biopsy is the gold standard - but it’s invasive. Only 5% of patients get one. Instead, doctors use blood markers like bone-specific alkaline phosphatase (BSAP) and PINP to estimate bone turnover. If BSAP is low and PTH is low? You likely have adynamic bone disease. If both are high? High turnover.
For vascular calcification, a simple chest X-ray can show signs. But CT scans (Agatston score) are more accurate. By Stage 4, 40% of patients already have detectable calcification. By dialysis? Up to 90%.
Treatment: It’s Not Just Pills
There’s no magic drug. Treatment is a balancing act - and it starts with diet.
Phosphate control is number one. You need to eat less than 800-1000 mg of phosphorus daily. That means avoiding processed foods, colas, and packaged meats. Natural foods like chicken or eggs have phosphorus too, but your body absorbs less of it. Processed foods? Nearly all of it gets absorbed. That’s why soda and deli meats are worse than steak.
Phosphate binders help. But not all are equal:
- Calcium-based binders (calcium acetate, carbonate): Effective, but don’t use more than 1500 mg elemental calcium per day. Too much = more calcification.
- Sevelamer (Renagel, Renvela): Non-calcium, non-aluminum. Better for arteries. But expensive. Dose: 2400-7200 mg/day.
- Lanthanum carbonate (Fosrenol): Also non-calcium. Chewable tablets. Dose: 750-3000 mg/day.
Vitamin D therapy: Start with cholecalciferol (D3) - 1000-4000 IU/day - to get your 25(OH)D above 30 ng/mL. Only use active forms (calcitriol, paricalcitol) if PTH is above 500 pg/mL and you’re not responding to binders and diet. Active forms raise calcium and phosphorus fast. Use them carefully.
Calcimimetics like cinacalcet or etelcalcetide help when PTH stays high despite everything else. Cinacalcet lowers PTH by 30-50%. Etelcalcetide (injectable) works even better - up to 45% reduction. Both avoid the calcium-phosphate spikes you get with vitamin D analogs.
And yes - dialysis matters. Four to five hours, three times a week. Shorter or less frequent sessions? Phosphorus builds up faster. It’s not just about cleaning blood. It’s about removing phosphate.
The New Thinking: Treat Early, Treat Together
The biggest shift in the last five years? CKD-MBD doesn’t wait until Stage 5. It starts in Stage 3.
FGF23 rises before phosphate does - by 5 to 10 years. That’s why the 2024 KDIGO draft recommends checking 25-hydroxyvitamin D every year once GFR drops below 60. And monitoring phosphate every 6-12 months, not just when you’re on dialysis.
Doctors now treat the whole syndrome - not just one number. You can’t fix PTH without fixing phosphate. You can’t fix phosphate without fixing vitamin D. And you can’t fix any of it without diet.
Children with CKD face a different battle: their bones can’t grow. Average height Z-scores are -1.5 to -2.0 SD below normal by Stage 5. That’s not just a number. That’s stunted growth. It’s why vitamin D and phosphate management in kids is aggressive - and non-negotiable.
What’s Next?
Researchers are testing new drugs. Anti-sclerostin antibodies like romosozumab are showing promise - they boost bone formation by 30-40% in early CKD. Klotho protein supplements, tested in animals, reduce vascular calcification by half. These aren’t available yet. But they’re coming.
One thing is clear: CKD-MBD is not a kidney problem. It’s a whole-body problem. And if you have chronic kidney disease, managing calcium, PTH, and vitamin D isn’t optional. It’s survival.


15 Comments
Reshma Sinha
December 12, 2025 AT 04:30CKD-MBD is a perfect storm of mineral dysregulation-phosphate toxicity, vitamin D resistance, and PTH runaway train. We need to treat this as a systems biology problem, not a lab value chase. FGF23 isn’t just a biomarker; it’s the canary in the coal mine. Early intervention with D3 and non-calcium binders? That’s where the real win is. Let’s stop waiting for dialysis to kick in before we act.
Lawrence Armstrong
December 13, 2025 AT 03:56So many people think low calcium = bad bones. But in CKD, it’s usually the opposite-your bones are leaking calcium to keep your blood stable. 😔 That’s why you need to look at BSAP and PINP, not just Ca++. Also, yes-dialysis duration matters. 3 hours? You’re just rinsing. 4.5+? That’s when phosphate actually leaves. 💪
Donna Anderson
December 14, 2025 AT 09:20Just read this and cried. My mom’s on dialysis and they never told her about the bone thing. She thought it was just ‘kidney stuff.’ Now I’m printing this out and taking it to her nephrologist. Thank you for explaining it like a human.
wendy b
December 15, 2025 AT 13:27Actually, the KDIGO guidelines are outdated. You know what the real issue is? Pharma. Calcium acetate is cheap. Sevelamer? That’s where the profit is. So they push binders that don’t even help with mortality. And vitamin D? They overprescribe active forms just to make PTH numbers look pretty. It’s not medicine-it’s accounting.
sandeep sanigarapu
December 16, 2025 AT 06:25Phosphate control is non-negotiable. Processed foods are poison. Eggs, chicken, lentils-fine. Cola, deli meat, instant noodles-death in disguise. Simple. No jargon needed.
Robert Webb
December 17, 2025 AT 07:12I’ve been managing my CKD for 12 years now, and the shift from focusing on PTH alone to understanding the whole triad-calcium, phosphate, vitamin D-was life-changing. I used to think if my PTH was under 300, I was fine. Turns out, my bone turnover was flatlining because I was on too much calcitriol and calcium binders. My doctor finally ordered a bone scan, and we switched to sevelamer and D3. My BSAP doubled in six months. It’s not magic-it’s balance. And yes, I still eat steak. Just not the processed kind.
nikki yamashita
December 19, 2025 AT 01:33YES! This is what we need to talk about more! My brother just started dialysis and they’re already giving him calcitriol. No diet talk. No binder options. Just pills. We need to push for education, not just prescriptions. 💪❤️
Adam Everitt
December 20, 2025 AT 09:05It’s ironic isn’t it? We treat the kidneys like they’re broken machines… but the real failure is systemic. The body’s trying to compensate… and we just throw drugs at it. FGF23? It’s not a villain-it’s a hero trying to save us from ourselves. And we respond by poisoning the system with calcium. We’re not healing. We’re just delaying the inevitable. Or are we?
Rob Purvis
December 21, 2025 AT 20:03Important note: Adynamic bone disease is underdiagnosed because we don’t check BSAP or PINP. If PTH is low and you’re on calcium binders? You’re probably in it. I’ve seen patients with dense, brittle bones on X-ray, but their doctors thought they were ‘doing great’ because their PTH was ‘normal.’ That’s a tragedy. Get a bone turnover marker test. Please.
Laura Weemering
December 22, 2025 AT 01:26So… who’s really behind this? Big Pharma? The nephrology guild? The dialysis corporations? They make billions off calcium binders and active vitamin D… and nobody talks about the fact that the real solution is… diet? And time? And not treating numbers? It’s all a racket. And they’re killing people with ‘care’.
Audrey Crothers
December 22, 2025 AT 13:39My aunt just got her first dialysis session and they didn’t even mention bone health. I’m so mad. 😤 I’m sending this to her doctor. You just explained it better than her nephrologist did in 30 minutes. Thank you. 🙏
Stacy Foster
December 23, 2025 AT 03:58They’re lying. They’ve been lying for decades. CKD-MBD isn’t a disease-it’s a profit model. They want you dependent on binders and injections. They don’t want you to know that eating real food and avoiding soda could have stopped this. And now you’re stuck. And they’re rich. It’s not medicine. It’s a scam.
Ashley Skipp
December 23, 2025 AT 10:34Why are we still using calcium binders? We know they calcify arteries. Why not just ban them? Simple answer: because they’re cheap and insurance won’t cover sevelamer. That’s not science. That’s capitalism.
Nathan Fatal
December 23, 2025 AT 23:20What fascinates me is how the body’s attempt to maintain homeostasis becomes its own destruction. PTH rises to save calcium. But in doing so, it hollows out the skeleton. Vitamin D deficiency triggers FGF23. FGF23 suppresses vitamin D. It’s a loop designed to kill. And yet-we’re still treating each piece like an isolated failure. We need to see the whole system. Not the numbers. The pattern.
Levi Cooper
December 25, 2025 AT 00:52My dad’s a veteran. Got kidney failure after Agent Orange exposure. They told him to eat less dairy. That’s it. No binders, no labs, no talk of bone disease. Meanwhile, in the VA system, they just pump him full of calcium pills. I’m not surprised. America treats kidneys like disposable parts. We don’t care about the whole body. Just the next bill.