Chronic diarrhea that won’t go away-no blood, no fever, no obvious cause-can be one of the most frustrating health problems. If you’ve been to the doctor multiple times, had normal colonoscopies, and still can’t figure out why you’re running to the bathroom 6 to 10 times a day, you might have microscopic colitis. It’s not flashy. It doesn’t show up on scans. But it’s real. And for thousands of people, especially women over 50, it’s the hidden reason behind their daily misery.
What Exactly Is Microscopic Colitis?
Microscopic colitis is an inflammatory condition of the colon that only shows up under a microscope. Unlike Crohn’s disease or ulcerative colitis, your colon looks perfectly normal during a colonoscopy. That’s why so many people go years without a diagnosis. The inflammation is invisible to the naked eye. You need biopsies-usually taken from multiple spots in the colon-to see the damage. There are two types: collagenous colitis and lymphocytic colitis. In collagenous colitis, a thick band of collagen-like scar tissue-builds up just beneath the colon lining. In lymphocytic colitis, there’s an overgrowth of white blood cells inside the lining. Both mess with the colon’s ability to absorb water, which is why diarrhea is always watery and never bloody. It’s not rare. About 5 out of every 100,000 people get diagnosed each year. Rates have more than quadrupled since the 1990s, mostly because doctors are better at testing for it. Women make up 65 to 70% of cases. Most people are diagnosed in their 60s. It’s not caused by diet or stress alone, though those can make symptoms worse.How Do You Know It’s Microscopic Colitis?
The symptoms are simple, but relentless:- Chronic watery diarrhea (5-10 bowel movements a day, often for months)
- Abdominal cramping or pain (about half of patients)
- Fecal incontinence (25-35% of people)
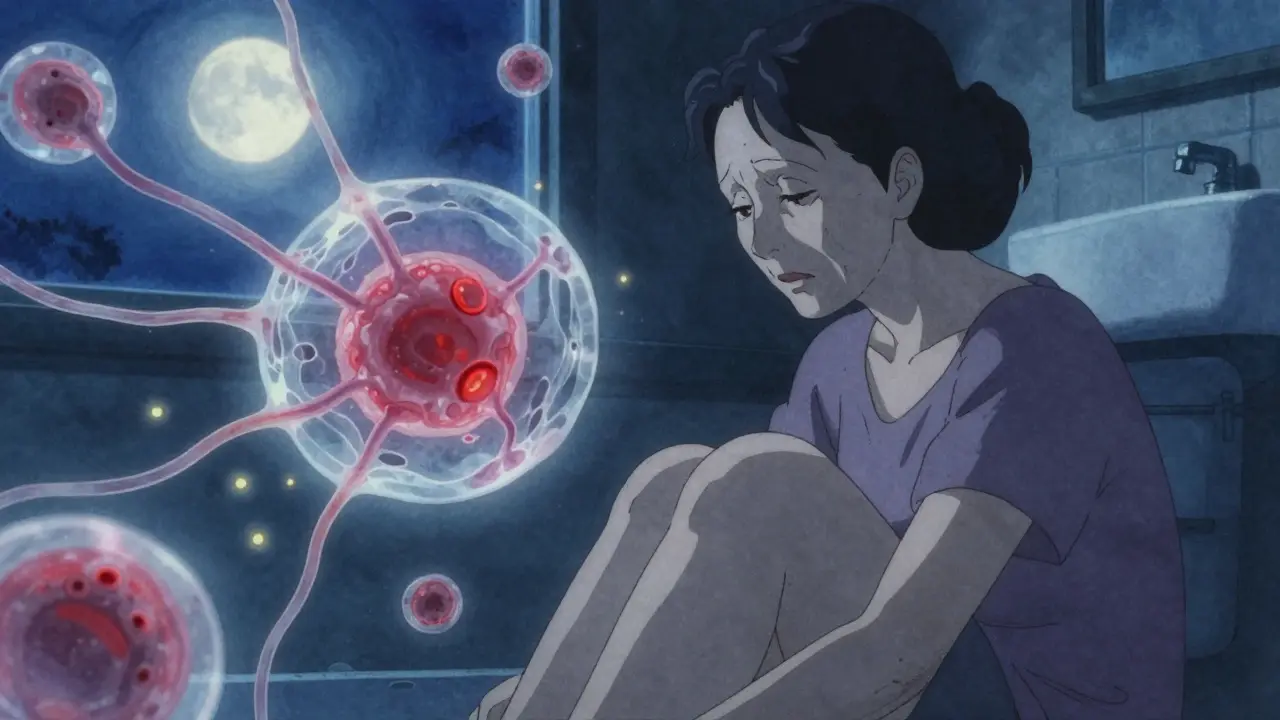
- Nocturnal diarrhea (you wake up at night to go)
- Unintentional weight loss (more common in collagenous colitis)
Why Budesonide Is the Gold Standard Treatment
For decades, doctors tried everything: fiber supplements, antidiarrheals, probiotics. Nothing worked reliably. Then came budesonide. Budesonide is a corticosteroid-but not like prednisone. It’s designed to work locally in the gut. When you swallow it, about 90% of it gets broken down by your liver before it enters your bloodstream. That means it shuts down inflammation in your colon without wrecking your bones, blood sugar, or sleep like traditional steroids do. Multiple clinical trials show budesonide works. In one study, 84% of collagenous colitis patients went into full remission after 8 weeks of 9mg daily. That’s compared to just 38% on placebo. For lymphocytic colitis, the numbers are similar: 75-85% response rate. Most people feel better within two weeks. Some say it’s like flipping a switch. The European Microscopic Colitis Group and the American College of Gastroenterology both give budesonide a strong, top-tier recommendation. It’s not just a guess-it’s backed by high-quality evidence from randomized trials.
How It’s Used: Dosing and Duration
The standard starting dose is 9mg per day, taken as a capsule, for 6 to 8 weeks. You don’t need to taper right away. After that, you stop. About 70-80% of people stay symptom-free for months. But here’s the catch: 50-75% come back after stopping. That’s where maintenance comes in. If your symptoms return, you might need to go back on budesonide-but at a lower dose: 6mg daily, or even 3mg every other day. Some people stay on low-dose budesonide for over a year. It’s not ideal, but it’s safer than going back to prednisone. Tapering slowly-cutting the dose by 3mg every 2-4 weeks-helps reduce relapse. Jumping off too fast? High chance of symptoms returning. Your doctor should guide this. Don’t self-adjust.What About Other Treatments?
Budesonide isn’t the only option, but it’s the best. Here’s how others stack up:- Bismuth subsalicylate (Pepto-Bismol): Works for about 26% of people. Cheap. Safe. But not strong enough for severe cases.
- Mesalamine: Used in ulcerative colitis. Only helps 40-50%. Not reliable for MC.
- Cholestyramine: Good if bile acid malabsorption is part of the problem. Works in 60-70% of those cases. Often combined with budesonide.
- Prednisone: Works as well as budesonide-but side effects are brutal. Weight gain, insomnia, high blood sugar, bone loss. Not worth it.
- Anti-TNF drugs (like infliximab): Expensive ($2,500 per infusion), risky for infection, and only help 20-30%. Reserved for when everything else fails.
Side Effects and Safety
Budesonide is safe-for most people. The most common side effects:- Insomnia (15%)
- Acne (12%)
- Mild mood changes or anxiety (8%)
- Headache or dizziness (rare)

Real People, Real Stories
On patient forums, the stories are split. About 68% say budesonide changed their life. One Reddit user wrote: “Went from 10 bathroom trips a day to 2 in 10 days. I hugged my wife for the first time in months.” But 32% report setbacks. Some relapse after stopping. Others can’t afford it. Generic budesonide costs $150-$250 for an 8-week course. Brand-name Entocort EC? $800-$1,200. Insurance often covers it, but not always. One patient on PatientsLikeMe said: “Worked great for 6 weeks. Then it stopped. Now I’m on maintenance for two years. I hate that I can’t stop.” Combination therapy helps some. Budesonide + cholestyramine fixed diarrhea for a woman who’d suffered for three years. It’s worth asking your doctor about.What’s Next for Treatment?
Research is moving fast. The FDA just gave vedolizumab fast-track status for microscopic colitis. It’s a biologic that targets gut-specific inflammation. Early results show 65% remission at 14 weeks. It’s not approved yet, but it’s coming. Scientists are also looking at genetics. Early data suggests people with the HLA-DQ2 or HLA-DQ8 genes respond better to budesonide. That could mean personalized treatment in the future: test your genes, then pick your drug. For now, budesonide remains the standard. It’s not perfect. It doesn’t cure the disease. But it gives people their lives back.What You Should Do If You Suspect Microscopic Colitis
If you’ve had chronic watery diarrhea for more than 3 months:- Ask your doctor for a colonoscopy with multiple biopsies-don’t accept a normal result unless they took at least four samples.
- If biopsies show microscopic colitis, ask about starting budesonide 9mg daily.
- Discuss a taper plan before you even start the medication.
- Get baseline blood work: HbA1c, blood pressure, bone density if you’re over 50.
- Consider adding cholestyramine if you have bile acid issues.
- Track your symptoms. Use a diary app. Note how many bowel movements, pain level, sleep quality.
Is microscopic colitis the same as IBS?
No. IBS is a functional disorder-your colon looks normal under a microscope. Microscopic colitis is an inflammatory disease that only shows up in biopsy samples. Both cause diarrhea, but IBS doesn’t involve immune system inflammation. You can’t diagnose microscopic colitis without a colonoscopy and biopsies.
Can you cure microscopic colitis?
There’s no known cure. But most people achieve long-term remission with treatment. About 25-30% never have symptoms again after stopping budesonide. The rest may need maintenance therapy or occasional short courses. It’s manageable, not fatal.
Why do women get microscopic colitis more often than men?
The exact reason isn’t clear, but hormones may play a role. Many women are diagnosed after menopause, when estrogen levels drop. Autoimmune conditions like collagenous colitis are more common in women overall. It’s not fully understood, but the link is strong.
Does diet affect microscopic colitis?
Diet doesn’t cause it, but it can trigger symptoms. Caffeine, dairy, artificial sweeteners, and fatty foods often worsen diarrhea. Some people benefit from a low-FODMAP diet. But unlike celiac disease, there’s no gluten trigger for most. Still, eliminating triggers can help reduce flare-ups.
Is budesonide safe for long-term use?
For most people, yes-especially at low maintenance doses (3-6mg daily). Studies show minimal systemic side effects even after 12-24 months. But long-term use requires monitoring: bone density scans, blood sugar checks, and blood pressure tracking. Your doctor should assess risks every 6-12 months.
How much does budesonide cost?
Generic budesonide costs $150-$250 for an 8-week course in the U.S. Brand-name Entocort EC can cost $800-$1,200. Insurance usually covers generic versions. In countries with public healthcare, it’s often low-cost or free. If cost is an issue, ask your doctor about patient assistance programs.


9 Comments
Raushan Richardson
December 27, 2025 AT 18:33I was diagnosed with collagenous colitis last year after 14 months of being told it was IBS. Budesonide was a godsend - I went from 8 trips a day to 2 in under two weeks. No more hiding during family dinners or canceling plans. I still take 3mg every other day as maintenance and it’s been stable for 10 months. If you’re suffering, don’t give up - get those biopsies.
Also, cholestyramine helped me with the lingering bile acid issue. Ask your doc about combining them.
Robyn Hays
December 29, 2025 AT 05:19Okay but can we talk about how wild it is that a disease with such a devastating impact on daily life - the sleepless nights, the anxiety of being far from a bathroom - was basically invisible to medicine until we started taking multiple biopsies? It’s like our bodies were screaming and doctors were just… not listening. And now we have a treatment that works without turning you into a zombie? That’s medical progress right there.
I also think the fact that it hits women over 50 so hard ties into how much we’ve been sidelined in medical research. Time to change that.
Anna Weitz
December 30, 2025 AT 03:42Budesonide isn’t magic it’s just better than the alternatives and yeah maybe we’re overmedicating but when you’re peeing yourself at 3am and your husband is sleeping on the couch because he can’t take it anymore you don’t care about side effects you care about being human again
dean du plessis
December 31, 2025 AT 04:25This is the kind of post that makes me grateful for the internet. I’m from South Africa and had never heard of microscopic colitis until now. The fact that it’s so common yet so underdiagnosed is shocking. I’ll be sharing this with my sister who’s had chronic diarrhea for years - she’s been told it’s stress. Maybe this will give her the push to ask for biopsies.
Kylie Robson
December 31, 2025 AT 10:47Technically speaking, budesonide’s first-pass hepatic metabolism results in a systemic bioavailability of approximately 9-12%, which is why its adverse effect profile is significantly attenuated compared to prednisone. The 9mg/day dosing regimen is supported by Phase III RCTs with a number needed to treat (NNT) of 2.1 for clinical remission at 8 weeks. The relapse rate post-taper is indeed 50-75%, which underscores the need for maintenance protocols. Also, the HLA-DQ2 association is statistically significant with p<0.01 in recent GWAS studies - this could enable precision medicine approaches within the next 5 years.
Caitlin Foster
January 1, 2026 AT 21:55So let me get this straight - you have a disease that makes you run to the bathroom 10 times a day, your colon looks ‘fine’ on a colonoscopy, so they just shrug and say ‘it’s IBS’... and then you take a pill that costs $200 and suddenly you’re human again? Why aren’t we screaming about this on national TV? Why isn’t this on the front page of every medical journal? I’m mad. And also… thank you.
Todd Scott
January 2, 2026 AT 08:50As someone who’s spent time in both the U.S. and India’s public health systems, I’ve seen how this disease slips through the cracks everywhere - but for different reasons. In the U.S., it’s overtesting and misdiagnosis - doctors assume IBS because it’s easier. In India, it’s under-testing - biopsies are expensive, and colonoscopies are often reserved for people with bleeding or weight loss. The fact that this condition is so prevalent among postmenopausal women speaks to a deeper gap in how we understand hormonal-immune interactions. I’ve had patients in Delhi who were on loperamide for 5 years before someone finally took four biopsies. One of them cried when she got the diagnosis. Not because she had a disease - but because she finally had an answer.
Chris Garcia
January 3, 2026 AT 03:05In many African cultures, bodily suffering is often framed as spiritual or karmic - something to endure rather than diagnose. But this condition doesn’t care about your beliefs. It doesn’t care if you’re spiritual or skeptical. It just takes your life, one bathroom trip at a time. The fact that budesonide works with such precision, with minimal systemic damage, is a quiet revolution. We need to bring this knowledge to rural clinics and community health workers. Not just in the West. Not just for the privileged. For every woman who wakes up in the dark, afraid to move too far from the toilet.
Elizabeth Ganak
January 3, 2026 AT 11:10my mom was diagnosed with this last year and budesonide saved her. she’s been on 3mg every other day for 8 months now and she’s back to gardening and traveling. we didn’t even know what to ask the doctor until i found this post. thank you.