For many people with diabetes, the biggest threat to their vision doesn’t come from blurry vision or floaters. It comes from silence. Diabetic retinopathy often creeps in without warning, slowly damaging the blood vessels in your retina until it’s too late. By the time you notice something’s wrong, the damage may already be severe. But here’s the truth: if you catch it early, you have a 95% chance of keeping your sight. That’s not a guess-it’s what doctors at UVA Health see in patients who get screened and treated on time.
What Exactly Is Diabetic Retinopathy?
Diabetic retinopathy is damage to the retina caused by high blood sugar over time. Your retina is the light-sensitive layer at the back of your eye. It turns light into signals your brain turns into images. When blood sugar stays high for years, it starts to wreck the tiny blood vessels that feed the retina. These vessels weaken, leak fluid, or get blocked. Sometimes, the eye tries to fix itself by growing new blood vessels-but these are fragile, messy, and prone to bleeding. That’s when things get dangerous. This isn’t just a complication of diabetes. It’s the leading cause of vision loss in adults between 21 and 64 in the U.S., according to the National Eye Institute. About one in three people with diabetes will develop some form of it. And the longer you’ve had diabetes, the higher your risk. Someone with Type 1 diabetes for 20 years? Their chance of retinopathy jumps to over 80%. For Type 2? It’s still around 60% after 15 years.The Three Stages of Retinal Damage
Diabetic retinopathy doesn’t jump from zero to blind overnight. It progresses in three clear stages:- Mild Nonproliferative Retinopathy: This is the earliest stage. Tiny bulges called microaneurysms form in the retinal blood vessels. They’re like weak spots in a garden hose. At this point, you won’t notice anything. No blurriness. No spots. Just silent damage.
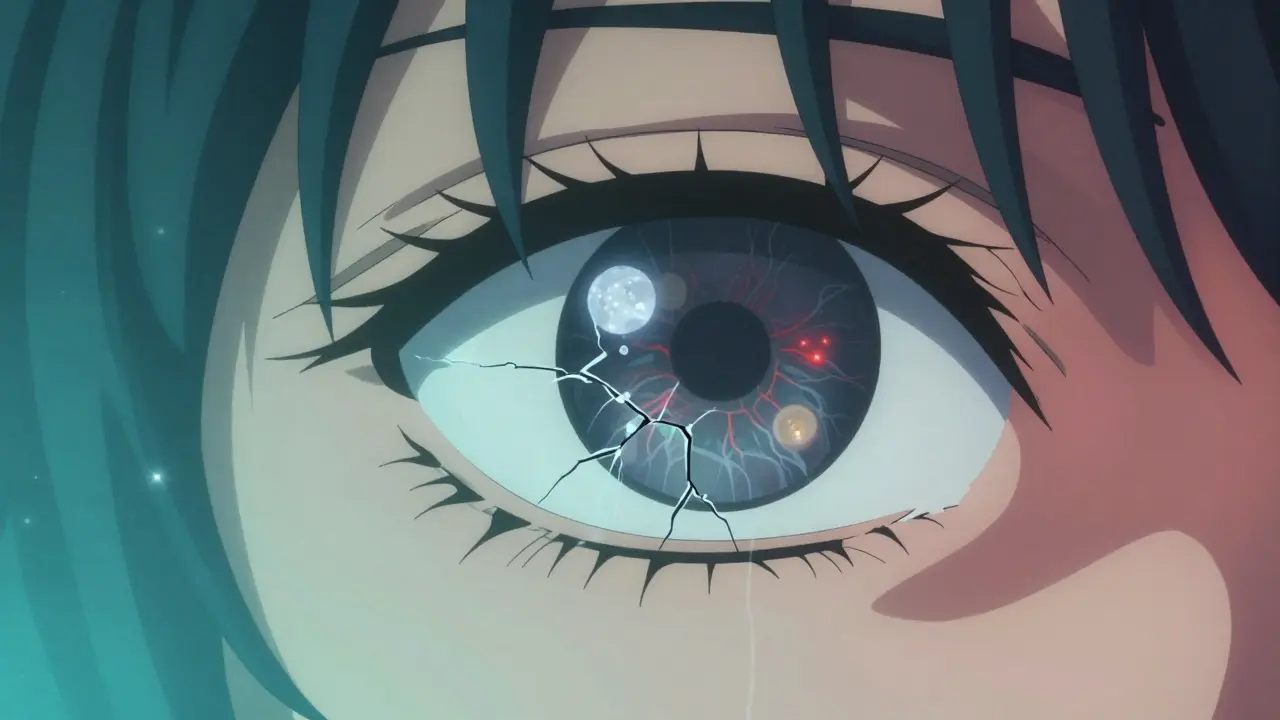
- Moderate to Severe Nonproliferative Retinopathy: More vessels get blocked. Blood flow to parts of the retina drops. The eye starts to swell, especially in the macula-the part responsible for sharp, central vision. This swelling is called diabetic macular edema (DME). About 1 in 15 people with diabetes will develop DME. Vision gets blurry, wavy, or distorted. Colors look faded.
- Proliferative Diabetic Retinopathy: This is the emergency stage. The retina isn’t getting enough oxygen. So it sends out signals to grow new blood vessels. These vessels are abnormal. They’re thin, leaky, and grow on the surface of the retina or into the vitreous gel inside your eye. They can bleed suddenly-causing dark floaters or even complete vision loss. They can also pull on the retina, causing it to detach. That’s a medical emergency.
Why You Might Not Notice Anything Until It’s Too Late
This is the cruel trick of diabetic retinopathy. You can have moderate damage and still read the clock, drive to the store, or watch TV. That’s why so many people don’t realize they have it until they wake up with floaters, or their vision suddenly goes dark. Studies show that 68% of patients only notice symptoms when the condition is already moderate or worse. The most common signs people report:- Floaters or dark spots that won’t go away (65% of cases)
- Blurred or wavy vision, especially when reading (78% in later stages)
- Difficulty seeing at night or in low light (52%)
- Fading or washed-out colors (41%)
- Loss of peripheral vision (37%)
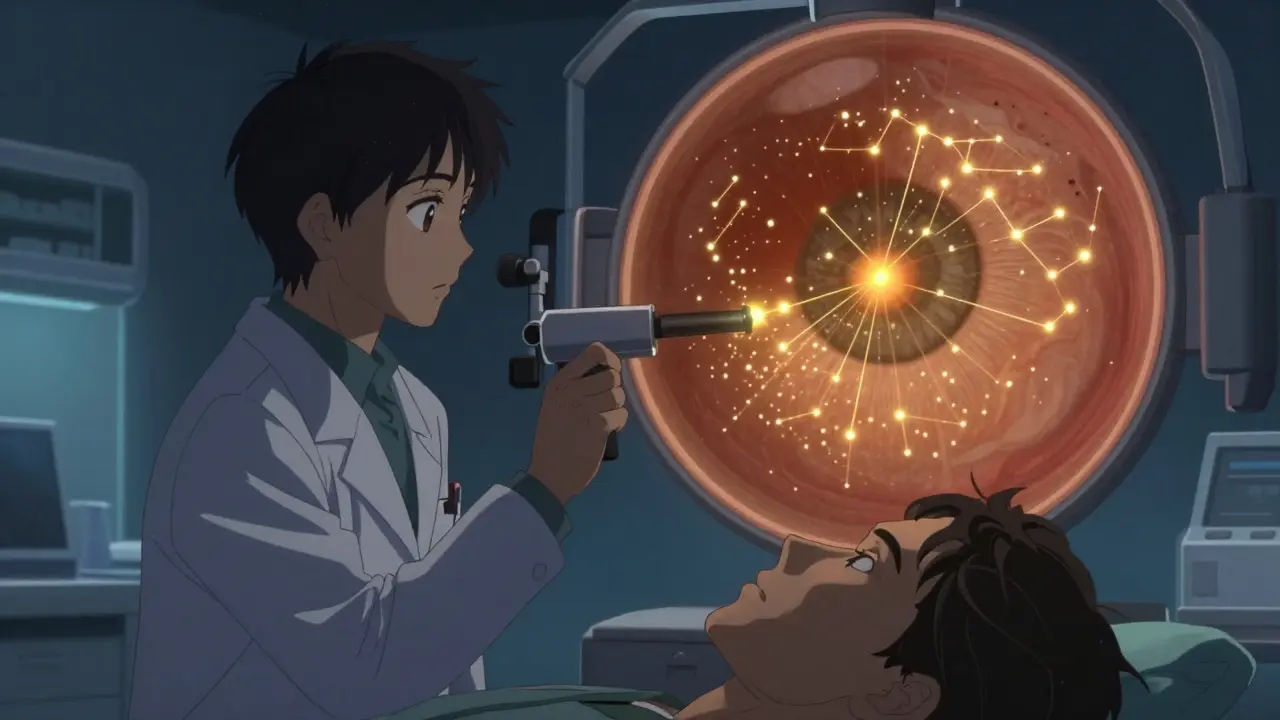
How Laser Treatment Works to Save Your Vision
Laser treatment, or photocoagulation, has been the backbone of diabetic retinopathy treatment for decades. It’s not glamorous. It’s not a cure. But it works. And when used at the right time, it can stop vision loss in its tracks. There are two main types:- Focal Laser Treatment: Used for diabetic macular edema. The doctor targets specific leaking blood vessels in the macula. The laser seals them off, reducing swelling. This doesn’t restore lost vision, but it stops it from getting worse. Most patients see stabilization-some even get slight improvement.
- Scatter Laser Treatment (Panretinal Photocoagulation): Used for proliferative retinopathy. Instead of targeting one spot, the laser makes hundreds of tiny burns across the peripheral retina. This doesn’t help your side vision much, but it reduces the eye’s signal to grow abnormal vessels. The goal? Starve the bad vessels so they shrink and stop bleeding.
What Else Helps? Blood Sugar, Blood Pressure, and Lifestyle
Laser treatment isn’t a magic fix. It’s one piece of a bigger puzzle. The real hero? Consistent blood sugar control. Research from the Cleveland Clinic shows that keeping your A1C below 7% slows retinopathy progression by up to 76%. That’s not a small number. That’s life-changing. But it’s not just sugar. High blood pressure and high cholesterol make retinal damage worse. Smoking? It doubles your risk of severe retinopathy. If you have diabetes, you need to treat your whole body-not just your eyes. That means:- Checking your blood sugar daily
- Taking medications as prescribed
- Eating a balanced diet low in refined carbs
- Exercising regularly
- Keeping your blood pressure under 130/80
- Quitting smoking
Screening: The Only Way to Catch It Early
The NHS and the American Diabetes Association both say: get a dilated eye exam every year. That’s non-negotiable. Even if your vision is perfect. Even if you feel fine. Even if you’ve had diabetes for only two years. A dilated eye exam means drops are put in your eyes to widen your pupils. That lets the doctor see the back of your retina clearly. They’re looking for microaneurysms, swelling, bleeding, or new vessels. It’s quick. It’s painless. It takes less than 15 minutes. Some clinics now use digital retinal imaging-no drops needed. You just look into a camera. It’s becoming more common, especially in rural areas. But if your doctor recommends dilation, don’t skip it. Digital images can miss early changes.
What’s Next? New Treatments on the Horizon
Laser treatment isn’t going away. But it’s no longer the only tool. Anti-VEGF injections-like ranibizumab and aflibercept-are now first-line for diabetic macular edema. These are shots into the eye that block the protein causing abnormal blood vessel growth and leakage. Many patients see better results with injections than with laser alone. Some doctors now combine laser with injections. That’s called combination therapy. It’s becoming the new standard for complex cases. Research is also moving toward AI-powered screening tools. In Australia, some telehealth programs now use AI to analyze retinal photos taken in GP clinics. If the AI spots signs of damage, you’re fast-tracked to an eye specialist. It’s not perfect yet-but it’s helping catch cases earlier, especially in places with few eye doctors.What Happens If You Don’t Treat It?
Left untreated, diabetic retinopathy doesn’t just blur your vision. It can steal it completely. Bleeding into the vitreous can cause sudden, permanent vision loss. Retinal detachment can lead to total blindness in that eye. Neovascular glaucoma-a rare but devastating complication-can destroy the eye’s drainage system, causing pressure to spike and nerves to die. And here’s the worst part: once photoreceptor cells (the light-sensing cells in your retina) die, they don’t come back. No laser. No injection. No surgery can bring them back. That’s why waiting is the most dangerous thing you can do.Final Reality Check
You don’t need to be perfect. You don’t need to have flawless blood sugar. But you do need to be consistent. You need to show up for your eye exams. You need to take your diabetes seriously-not just for your kidneys or your feet, but for your eyes. The data is clear: if you have diabetes, your eyes are at risk. But if you get screened, manage your health, and act early, you can live a full life without losing your sight. That’s not hope. That’s science.Can diabetic retinopathy be reversed?
Early damage can be stabilized and sometimes improved with treatment, but once photoreceptor cells in the retina die, the damage is permanent. That’s why early detection is critical-laser and injections can stop further loss, but they can’t restore vision that’s already gone.
How often should I get my eyes checked if I have diabetes?
If you have any type of diabetes, you need a dilated eye exam at least once a year. If you already have retinopathy, your doctor may recommend exams every 3 to 6 months. Pregnant women with diabetes should be checked in the first trimester and monitored closely throughout pregnancy.
Is laser treatment painful?
Most people feel only mild discomfort, like pressure or brief flashes of light. Numbing drops are used, and the procedure is quick-usually under 30 minutes. Some mild blurriness or light sensitivity afterward is normal, but serious pain is rare.
Can I drive after laser treatment?
Not right away. The dilating drops used during the exam can blur your vision for several hours. You’ll need someone to drive you home. Some people also experience temporary glare or reduced night vision after laser treatment, so avoid driving at night for a few days until your eyes adjust.
Do I still need laser treatment if I’m getting eye injections?
It depends. For diabetic macular edema, injections are often the first choice. But if swelling comes back or doesn’t respond well, laser may be added. For proliferative retinopathy, laser is still the main treatment, though injections can help reduce bleeding and swelling. Many patients now get a combination of both.
Are there alternatives to laser treatment?
Yes. Anti-VEGF injections are now preferred for macular edema. In severe cases, a vitrectomy-surgery to remove blood from the vitreous-may be needed. But laser remains essential for preventing new vessel growth in advanced stages. The best approach often combines multiple treatments.


14 Comments
kumar kc
January 20, 2026 AT 12:23Stop ignoring your eyes. If you have diabetes, you’re already risking blindness. No excuses. Get checked.
Carolyn Rose Meszaros
January 21, 2026 AT 00:04This hit me hard 😢 I’ve had Type 2 for 12 years and never thought my eyes were at risk… I booked my dilated exam today. Thanks for the wake-up call. 🙏
Greg Robertson
January 21, 2026 AT 07:27Really appreciate how clear this breakdown is. I’ve seen friends brush off eye exams because ‘they can still see fine’ - this is exactly the kind of info that changes minds. Thanks for sharing.
Jacob Cathro
January 23, 2026 AT 02:40laser treatment? lol. they just burn your retina like a damn toaster. 95% success? more like 95% of people are too scared to ask what else they're hiding. next thing you know, they're injecting you with 'anti-vegf' that costs 2k a shot. big pharma loves diabetics. 💸
Paul Barnes
January 23, 2026 AT 23:30The data presented here is statistically sound and clinically validated. The claim of 95% vision preservation with timely intervention is supported by multiple longitudinal studies, including the DCCT and UKPDS. It is not hyperbole; it is evidence-based medicine.
pragya mishra
January 25, 2026 AT 19:24Why are you only talking about laser and injections? What about natural remedies? Turmeric, cinnamon, bitter melon? I’ve seen people reverse their diabetes with diet alone - why won’t doctors tell you this? They want you dependent on their treatments!
Manoj Kumar Billigunta
January 26, 2026 AT 08:04Hey, if you're reading this and you have diabetes - you're not alone. I’ve been there. I had retinopathy in my 40s, got laser, tightened my diet, lost 40 pounds, and now my A1C is 5.8. It’s not about being perfect. It’s about showing up. One exam. One healthy meal. One walk. Start there. You got this.
sagar sanadi
January 27, 2026 AT 23:46Wait… so you're telling me the government and the eye doctors are telling the truth? That’s weird. I thought they were all in on the diabetes scam with the insulin and the eye drops and the ‘annual exams’ to keep us paying. I’m gonna skip my appointment and just stare at the sun instead. Free vision therapy.
Nadia Watson
January 29, 2026 AT 06:35Thank you for this comprehensive and deeply informative overview. The integration of clinical data with practical guidance is both rare and invaluable. I shall be sharing this with my diabetes support group in Atlanta. Your clarity is a gift.
Thomas Varner
January 30, 2026 AT 21:39I’ve had diabetic retinopathy since 2019… got the laser, then the injections, then the second laser… now I’m on my third round of anti-VEGF. It’s not fun, but I can still see my granddaughter’s face. That’s worth every flash, every drop, every $2,000 shot. Don’t wait. Don’t gamble. Do the work.
Art Gar
January 31, 2026 AT 13:57The assertion that early detection yields a 95% preservation rate is misleading. The population studied was highly compliant, with access to consistent care. This statistic is not generalizable to underserved communities, where screening rates remain below 40%. The article omits systemic inequities.
Edith Brederode
February 1, 2026 AT 04:48My mom had this and lost her vision in one eye before she got treated… I cried reading this. I just scheduled her next appointment. Thank you for writing this. 💕
clifford hoang
February 3, 2026 AT 01:58What if the retina damage isn't from sugar at all? What if it's from the glyphosate in our food? Or the 5G towers that fry our optic nerves? The doctors won't tell you this because they're paid by Monsanto and the telecom giants. Laser? Nah. We need detox protocols and orgone generators. 🌿📡👁️
Arlene Mathison
February 4, 2026 AT 02:48You can beat this. I was told I’d be blind by 50. I’m 53. I see my kids’ graduations. I read bedtime stories. I drive to the grocery store. It’s not easy - but it’s possible. Get the exam. Take the meds. Walk after dinner. One day at a time. You’re stronger than you think.