What Are CGRP Inhibitors and Why Do They Matter?
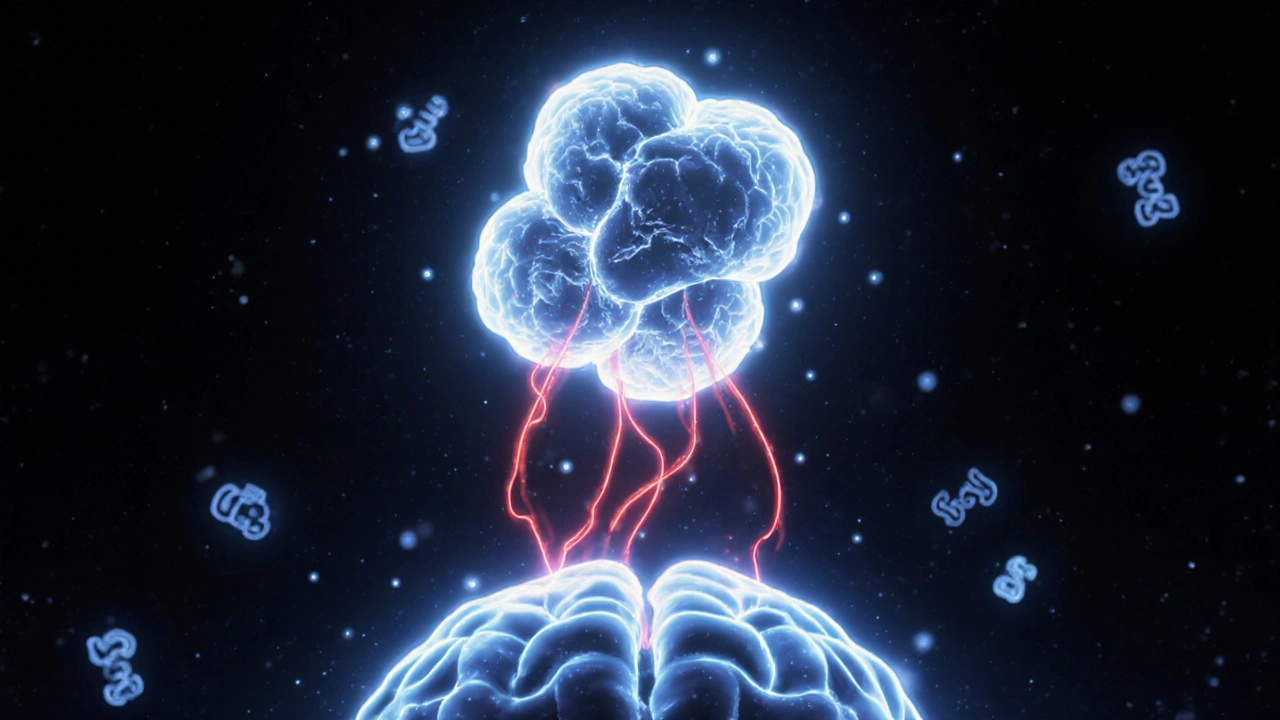
Before 2018, if you had migraines, your doctor had few options that actually targeted the root cause. Most preventive meds were repurposed drugs - antidepressants, blood pressure pills, or seizure medications - originally designed for something else entirely. Then came CGRP inhibitors: the first class of drugs made specifically for migraine prevention. They don’t just mask symptoms. They block a key player in migraine attacks: calcitonin gene-related peptide, or CGRP.
CGRP is a protein that floods the brain during a migraine, triggering inflammation, pain signals, and blood vessel swelling. By stopping CGRP from doing its job, these drugs cut the migraine cycle at the source. The American Migraine Foundation called them "the biggest news in migraine treatment in decades," and for good reason. For the first time, people with chronic migraines aren’t just managing pain - they’re reclaiming their lives.
How Do CGRP Inhibitors Work?
There are two main types of CGRP inhibitors: monoclonal antibodies (mAbs) and gepants. Both block CGRP, but they do it in different ways.
Monoclonal antibodies - like erenumab (Aimovig), fremanezumab (Ajovy), galcanezumab (Emgality), and eptinezumab (Vyepti) - are large protein molecules. They’re injected under the skin (or infused intravenously) and work by either grabbing onto the CGRP protein itself or locking onto its receptor so the signal can’t get through. These are used for prevention only. You get them once a month or once every three months.
Gepants - like rimegepant (Nurtec ODT), ubrogepant (Ubrelvy), and zavegepant (Zavzpret) - are smaller pills or nasal sprays. They block the CGRP receptor too, but they’re fast-acting. Rimegepant is approved for both preventing migraines (taken every other day) and stopping one in progress. That’s huge. It’s the first drug that can do both.
Unlike triptans, which narrow blood vessels and can be dangerous for people with heart disease, CGRP inhibitors don’t affect circulation. That makes them safer for a lot of patients who’ve been told they can’t use older migraine meds.
Who Benefits Most From CGRP Inhibitors?
These drugs aren’t magic bullets for everyone - but they work incredibly well for specific groups.
People with chronic migraine (15 or more headache days a month) see the biggest gains. In clinical trials, 84% of chronic migraine patients had fewer headache days. Many drop from 20 days a month to 5 or fewer. One patient on Drugs.com wrote: "After 15 years of chronic migraine, Emgality got me down to episodic in 3 months. Life-changing."
They also help those with medication overuse headache - when taking painkillers too often makes migraines worse. CGRP inhibitors break that cycle without adding more drugs to the mix.
Patients who’ve tried and failed at least two other preventives - like topiramate or propranolol - still respond well. About 30% of people who had no luck with older meds saw at least a 50% drop in migraine days with CGRP inhibitors.
Even people with migraine with aura (visual disturbances before the headache) respond. That’s rare. Most older preventives don’t help aura at all.
How Effective Are They Really?
Let’s talk numbers. In head-to-head studies, erenumab outperformed topiramate: 41% of patients on erenumab cut their migraine days by half or more. Only 24% did on topiramate. That’s a big difference.
Overall, about half of all users see a 50% or greater reduction in migraine days. For some, it’s even better. In a 2023 survey of 1,247 patients on Migraine.com, 78% said CGRP inhibitors were "very effective" or "effective." On Reddit’s r/migraine community, 82% of posts were positive.
Real-world results match clinical trials. One patient on Aimovig wrote: "Went from 20 migraine days to 5. I can now work full-time again."
And the effects add up. If you used to get eight migraine days a month, you’re likely to drop to four or fewer. That’s not just less pain - it’s more time with family, more productivity, fewer ER visits.
How Are They Taken? Injections, Pills, or Sprays?
Delivery matters. If you hate needles, you have options.
- Monthly injections: Erenumab (70mg or 140mg), fremanezumab (225mg), galcanezumab (120mg). All self-administered with a small pen.
- Quarterly injections: Fremanezumab (675mg every 3 months), eptinezumab (100mg or 300mg via IV infusion every 3 months).
- Oral pills: Rimegepant (75mg every other day for prevention), ubrogepant (50mg or 100mg as needed for attacks).
- Nasal spray: Zavegepant (10mg) - fast relief in under 30 minutes, approved for acute treatment.
No one size fits all. Some patients prefer the convenience of a monthly shot. Others like the flexibility of a pill they can take only when they feel a migraine coming on. Rimegepant is the only one approved for both prevention and acute use - a game-changer for people who want one tool for everything.
Cost and Insurance: What You Need to Know
These drugs are expensive. Monoclonal antibodies cost $650-$750 a month. Gepants run $800-$1,000. That’s three to five times more than generic preventives like propranolol or topiramate.
But here’s the catch: most U.S. insurance plans cover them - if you jump through the right hoops. Prior authorization is almost always required. About 35% of initial requests get denied. That’s frustrating, but it’s not the end.
Manufacturers offer patient assistance programs that cover 80% of out-of-pocket costs for eligible people. Many also have 24/7 nurse hotlines to help with paperwork. Websites like AimovigSupport.com and EmgalityConnect.com walk you through the process step by step.
One patient shared: "My insurance denied me twice. I called the manufacturer’s support line. They mailed me a free 3-month supply while we appealed. Got approved on the third try."
For many, the cost is worth it. When you’re missing work, canceling plans, and relying on painkillers daily, $700 a month can feel like a bargain.
Side Effects and Safety
Compared to older preventives, CGRP inhibitors are remarkably safe.
Common side effects? Injection site reactions - redness, itching, or pain - affect about 28% of users. That’s usually mild and fades over time. Constipation happens in a small number of people on erenumab, but it’s rarely severe.
Unlike topiramate (which can cause brain fog, weight loss, or kidney stones) or beta-blockers (which can cause fatigue or low blood pressure), CGRP inhibitors don’t affect your thinking, mood, or heart rhythm.
One concern with gepants: liver enzyme changes. The FDA requires monitoring for ubrogepant and rimegepant, especially if you’re on other medications that affect the liver. But serious liver damage is extremely rare.
Long-term data beyond five years is still limited. But in clinical trials, only 0.8% of patients stopped treatment because of side effects. That’s lower than almost any other preventive.

How Do They Compare to Old-School Preventives?
Here’s a quick breakdown:
| Feature | CGRP Inhibitors | Traditional Preventives (e.g., Topiramate, Propranolol) |
|---|---|---|
| Targeted to migraine? | Yes | No - repurposed from other conditions |
| Effectiveness (≥50% reduction) | ~50% of patients | ~30-40% of patients |
| Works for medication overuse? | Yes | Usually not |
| Cardiovascular safety | Safe - no vasoconstriction | Caution needed - beta-blockers can lower BP |
| Side effect profile | Mild - mostly injection site reactions | Common - brain fog, weight changes, fatigue |
| Dosing frequency | Monthly, quarterly, or every other day | Daily pill |
Doctors now see CGRP inhibitors as first-line treatment - no need to try and fail on older drugs first. The American Headache Society’s 2023 guidelines say they should be "considered a first-line treatment option for migraine prevention." That’s a huge shift.
What’s Next? The Future of CGRP Therapy
The field is moving fast. Researchers are testing:
- Combination therapy: Using CGRP inhibitors with Botox. One study showed 63% of patients hit a 50% reduction with both - compared to 41% with either alone.
- Pediatric use: Erenumab trials in teens are complete. Approval for adolescents could come by 2026.
- New delivery methods: Nasal sprays and patches are in development to make treatment even easier.
- Expanded uses: Trials are underway for vestibular migraine and post-traumatic headache.
By 2030, experts predict CGRP inhibitors will be the standard of care. The only real hurdle? Cost. Insurance systems aren’t built for $700-a-month drugs. But as more data comes in and generics (biosimilars) arrive after 2028, prices should drop.
Getting Started: What to Do Next
If you’re considering CGRP inhibitors:
- Confirm your diagnosis. You need at least 4 migraine days a month to qualify.
- Talk to a neurologist or headache specialist. Primary care doctors can prescribe them, but specialists have more experience.
- Check your insurance coverage. Ask about prior authorization requirements.
- Use manufacturer support programs. They’ll help with paperwork and may give you free samples.
- Give it time. It can take 2-3 months to see full results.
Don’t give up if your first request is denied. Appeals work. Many patients get approved on the second try.
Final Thoughts
CGRP inhibitors aren’t perfect. They’re expensive. They require injections or pills. They don’t work for everyone. But they’re the first real breakthrough in migraine prevention in over 30 years. For millions of people who’ve spent years trying pills that didn’t work or caused side effects, these drugs offer something rare: hope with real results.
If you’re tired of living in the shadow of migraine pain, it’s time to ask your doctor about CGRP inhibitors. You might be one appointment away from a life with fewer headaches - and more moments that matter.


15 Comments
Andrew McAfee
November 24, 2025 AT 11:22Been on Aimovig for 8 months now. Used to get 20 migraines a month. Now I'm at 3. I actually made it to my niece's wedding without hiding in a dark room. Life's weird like that.
Andrew Camacho
November 25, 2025 AT 14:04I mean sure it works but have you seen the price tag? $700 a month? That's like buying a new phone every month and calling it healthcare. The pharmaceutical industry is running a scam and we're all just sheep waiting for the next injection.
Arup Kuri
November 27, 2025 AT 13:30They say it blocks CGRP but what about the other 47 proteins they ignore? This is just another western placebo dressed up in lab coats. In India we use turmeric and yoga and we don't need these fancy pills to live
Elise Lakey
November 27, 2025 AT 21:51I'm curious how long the long-term effects last? I've heard some people stop and then migraines come back worse. Is that common? I just want to know if this is a bandaid or a cure.
Erika Hunt
November 29, 2025 AT 13:22I think it's incredible that we've finally moved beyond repurposing drugs designed for epilepsy or hypertension to actually targeting the biological mechanism of migraine... it's not just about pain relief anymore, it's about neurology, it's about understanding the brain's signaling pathways, it's about precision medicine finally catching up to what patients have been screaming about for decades, and honestly, it gives me hope that maybe one day we'll stop treating symptoms and start treating causes, even if it's still expensive and insurance is a nightmare, the science is finally on our side.
prasad gaude
December 1, 2025 AT 13:09You know, back in my village in Kerala, we used to say pain is just the body knocking. Now we knock back with billion-dollar drugs. I wonder if we're healing or just silencing the message.
Timothy Sadleir
December 2, 2025 AT 10:12The data presented here is statistically significant but lacks longitudinal peer-reviewed validation beyond five years. Furthermore, the reliance on self-reported outcomes from non-blinded patient surveys introduces significant selection bias. One must consider the placebo effect, especially in conditions with high psychosomatic components such as migraine.
Srikanth BH
December 4, 2025 AT 02:59If you're thinking about trying these, don't stress if your insurance says no at first. I got denied twice too. Called the Emgality hotline, they mailed me a free month and walked me through the appeal. Took 3 weeks. Now I'm down to 2 migraines a month. You got this.
Jennifer Griffith
December 5, 2025 AT 19:11so like... these things are just fancy botox right? i mean i heard they just numb your brain or something idk
Roscoe Howard
December 6, 2025 AT 18:33It's no surprise that American pharmaceutical companies have monopolized migraine treatment. In other countries, they use natural remedies. Here, we pay $700 for a shot and call it progress. This is capitalism disguised as medicine.
Kimberley Chronicle
December 8, 2025 AT 16:30The pharmacokinetic profile of gepants is particularly compelling given their reversible CGRP receptor antagonism and hepatic metabolism via CYP3A4, which necessitates careful polypharmacy management. The dual indication of rimegepant for acute and preventive use represents a paradigm shift in therapeutic architecture.
Shirou Spade
December 9, 2025 AT 09:26I think the real question isn't whether it works, but why it took us this long to figure out that pain isn't just something to endure. Maybe we were too busy fixing blood pressure to listen to the brain.
Lisa Odence
December 10, 2025 AT 04:54I've been on Nurtec for 6 months and it's literally changed my life 🌟 I went from missing 3 workdays a week to working full time 💼 I even started hiking again 🥾 The only downside? The cost 😭 But the manufacturer gave me a coupon and now I pay $20/month 😍 #CGRPRevolution #MigraineWarrior
Patricia McElhinney
December 10, 2025 AT 16:17The data is cherry-picked. Only 50% respond? That means half of patients are still suffering. And the constipation side effect? That's not 'mild'-it's debilitating. This is not a breakthrough-it's a marketing campaign dressed in white coats.
Dolapo Eniola
December 11, 2025 AT 21:38America always thinks money solves everything. In Nigeria we use prayer and cold compresses. These drugs are just for people who don't believe in God. You spend $700 and still get headaches? That's weak.