Delirium Risk Assessment Tool
Risk Assessment
When an older adult gets a urinary infection or pneumonia, doctors often reach for fluoroquinolones. These antibiotics-like levofloxacin and a class of broad-spectrum antibiotics that inhibit bacterial DNA replication-work fast, cover many bugs, and seem like a safe bet. But for people over 65, especially those with kidney issues or memory problems, these drugs can trigger something far more dangerous than a stomach upset: sudden, terrifying confusion known as delirium an acute state of confusion, disorientation, and altered awareness, often reversible.
What Does Fluoroquinolone-Induced Delirium Look Like?
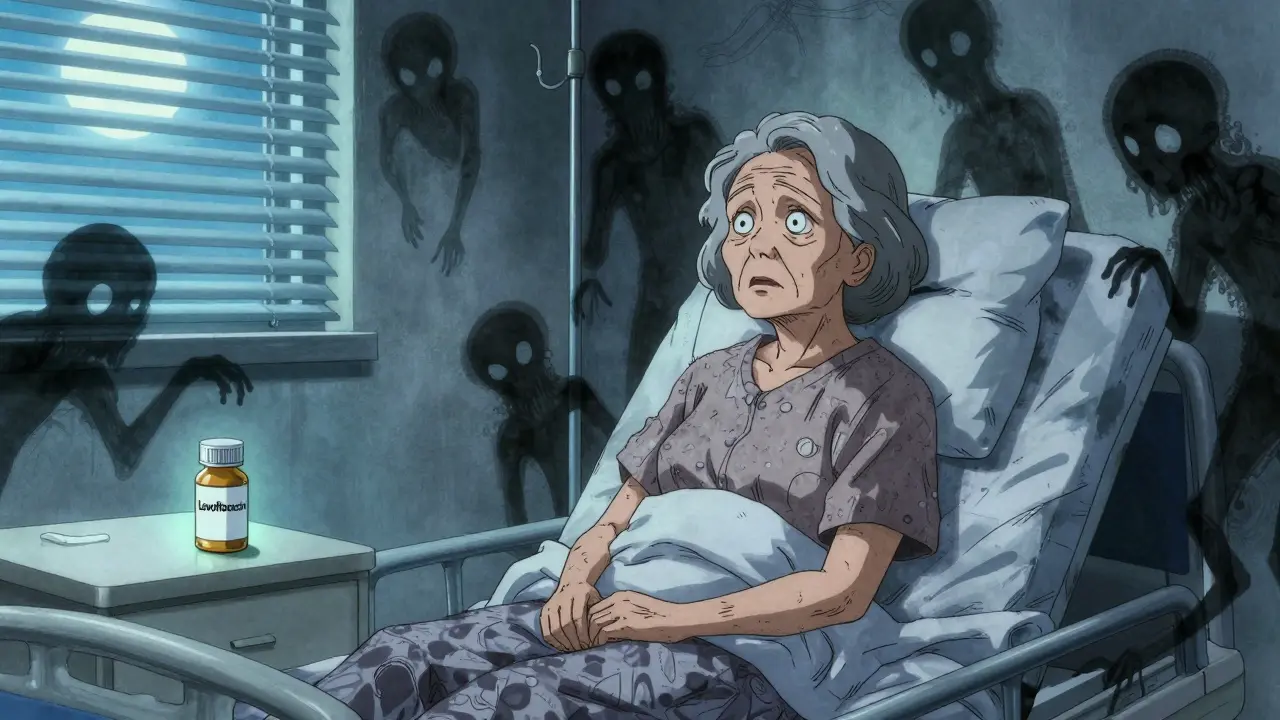
It doesn’t come on slowly. One day, your parent or grandparent is fine. The next, they’re staring blankly, forgetting where they are, or seeing things that aren’t there. They might hear voices. They become agitated, irritable, or completely withdrawn. They can’t focus on a simple conversation. Time and place lose meaning. This isn’t dementia. This is delirium-a medical emergency that can develop within 24 to 72 hours of starting the antibiotic.
A real case from a 2018 report described an 82-year-old woman who started levofloxacin a fluoroquinolone antibiotic commonly prescribed for urinary and respiratory infections for a bladder infection. On day three, she became confused, hallucinated shadows moving across the walls, and couldn’t recognize her own daughter. Her EEG and brain scan were normal. Her blood sugar and electrolytes? Fine. The only change? The antibiotic. Once stopped, her symptoms vanished in under 48 hours.
This isn’t rare. A 2016 review of nearly 400 cases of antibiotic-related delirium found that fluoroquinolones a class of antibiotics including ciprofloxacin, levofloxacin, and moxifloxacin were responsible for 18% of cases-more than any other class except vancomycin. And while overall rates are low, under 0.5% of users, the impact is huge. Older adults with delirium are more likely to end up in a nursing home, stay longer in the hospital, or even die.
Why Does This Happen?
It’s not just about aging. It’s about chemistry. Fluoroquinolones slip easily into the brain. Levofloxacin reaches 50-90% of the blood’s concentration in spinal fluid. Once inside, they interfere with GABA, the brain’s main calming chemical. Think of GABA as the brakes on your nervous system. When fluoroquinolones block it, your brain gets overexcited. This imbalance can trigger hallucinations, seizures, and confusion.
There’s more. These drugs also overstimulate NMDA receptors-another pathway that can push neurons into overdrive. The result? A neurological storm. This is why even healthy-looking older adults can crash mentally after just a few doses. The risk spikes with higher doses. A 750 mg daily dose of levofloxacin is twice the usual amount-and doubles the chance of delirium.
Who’s at Risk?
Not everyone gets this. But certain people are sitting ducks:
- Age 65+: Nearly half of hospitalized adults over 65 develop some form of cognitive disruption when on these drugs.
- Kidney problems: About 85% of levofloxacin leaves the body through the kidneys. If kidneys are weak, the drug builds up. A creatinine clearance below 50 mL/min is a red flag.
- Pre-existing brain issues: Mild cognitive impairment, early Alzheimer’s, or past strokes make the brain far more vulnerable.
- Dehydration or electrolyte imbalance: These make the brain’s chemistry even more unstable.
- Multiple medications: Mixing fluoroquinolones with steroids, antipsychotics, or even some heart drugs increases risk.
And here’s the kicker: many doctors don’t think of antibiotics when someone gets confused. They check for strokes, infections, or dementia. They miss the obvious: the new pill they just prescribed.
How Is It Diagnosed?
Delirium isn’t a lab test. It’s a clinical diagnosis. The DSM-IV criteria standard diagnostic guidelines for psychiatric conditions including delirium say you need:
- Sudden onset (hours to days)
- Fluctuating symptoms (better in morning, worse at night)
- Inability to focus attention
- Either disorganized thinking or altered consciousness
Doctors rule out other causes: normal brain scans, normal blood work, no signs of stroke or infection. If the patient started a fluoroquinolone within the last three days? That’s your clue.
What Should Be Done?
Stop the drug. Immediately.
That’s step one. No waiting. No waiting for a second opinion. No hoping it’ll pass. If delirium shows up after starting a fluoroquinolone, the antibiotic must be discontinued right away. Symptoms usually lift within 48 to 96 hours. In most cases, full recovery happens. But delay? That’s when complications pile up-falls, longer hospital stays, permanent cognitive decline.
Then, switch to a safer antibiotic. Beta-lactams like amoxicillin or cefazolin are usually fine. They don’t cross the blood-brain barrier as easily. Even cefepime a fourth-generation cephalosporin with potential neurotoxicity risk can cause issues, but it’s far less likely than levofloxacin.

What’s Changing in Practice?
The FDA didn’t wait. In July 2018, they forced drugmakers to update labels to include delirium as a known risk. The warning now says fluoroquinolones can cause disturbances in attention, memory loss, and serious mental disturbances.
And it’s working. After the 2018 alert, prescriptions for older adults dropped by over 20%. Hospitals like UCSF cut levofloxacin use for simple UTIs by 35% after implementing new protocols. The American Geriatrics Society now lists fluoroquinolones as potentially inappropriate for seniors in their 2023 Beers Criteria.
But here’s the problem: they’re still being prescribed. In 2019, over 26 million fluoroquinolone prescriptions were filled in the U.S. Many are for infections that could be treated with something safer-like a simple amoxicillin for a urinary infection. The CDC says fluoroquinolones should be reserved for infections with no other options. That’s not happening enough.
What Can You Do?
If you’re caring for an older adult:
- Ask: "Is this antibiotic necessary? Are there safer alternatives?"
- Check: "Do they have kidney issues? Have they had memory problems before?"
- Watch: "Are they confused, hallucinating, or acting strangely after starting this drug?"
- Act: "Call the doctor immediately if symptoms appear-don’t wait."
Don’t assume confusion is "just aging." It might be the antibiotic. And if it is, stopping it fast can mean the difference between going home-or ending up in a nursing home.
What About Future Treatments?
Researchers are looking at ways to predict who’s at risk. Early studies are testing biomarkers in blood or urine that might flag vulnerability before symptoms start. Some are designing new fluoroquinolone versions that don’t cross into the brain. Others are building smart alerts into electronic health records that flag high-risk patients before a script is even written.
But right now? The safest strategy is simple: avoid fluoroquinolones in older adults unless there’s no other choice. And if they’re given? Monitor like your life depends on it-because for many, it does.
Can fluoroquinolones cause permanent brain damage in older adults?
In most cases, no. Fluoroquinolone-induced delirium is usually reversible. Symptoms typically clear within 48 to 96 hours after stopping the drug. But if delirium isn’t recognized quickly, it can lead to falls, prolonged hospital stays, or complications like pneumonia or blood clots-which can cause lasting harm. While the cognitive effects themselves are not permanent, the consequences of delayed treatment can be.
Are all fluoroquinolones equally risky?
No. Levofloxacin and ciprofloxacin have the most documented cases of delirium in older adults. Moxifloxacin and gemifloxacin are also linked, but less frequently. The risk depends on how easily the drug crosses into the brain and how strongly it blocks GABA receptors. Levofloxacin, in particular, has high brain penetration and is commonly prescribed at higher doses (750 mg), which increases risk.
Why are older adults more vulnerable to these side effects?
Aging reduces kidney function, so drugs like levofloxacin build up in the body. The blood-brain barrier also weakens, letting more drug enter the brain. Older brains have fewer GABA receptors and less ability to compensate for chemical imbalances. Plus, many seniors take multiple medications that interact, making the brain more sensitive to disruption.
Can fluoroquinolones cause delirium in younger people?
Yes, but it’s much rarer. Younger people with healthy kidneys and no neurological history rarely develop delirium from these drugs. Cases in younger adults usually involve high doses, pre-existing mental health conditions, or severe kidney impairment. The risk is highest in those over 65.
What antibiotics are safer alternatives for older adults?
For common infections like urinary tract infections or pneumonia, beta-lactams are preferred: amoxicillin, ampicillin, cefazolin, or ceftriaxone. These have minimal brain penetration and don’t interfere with GABA. For some infections, trimethoprim-sulfamethoxazole or nitrofurantoin may be options. Always ask: "Is there a safer antibiotic that works just as well?"


8 Comments
Prateek Nalwaya
February 15, 2026 AT 15:01Man, I never thought about antibiotics causing hallucinations. My dad was on levofloxacin for a UTI last year and started talking to invisible people - we thought he was having a stroke. Turned out it was the drug. Docs didn’t even blink. This post is a godsend. We need way more awareness. It’s wild how we treat older folks like walking pharmacies.
Jonathan Ruth
February 16, 2026 AT 11:41Fluoroquinolones are overprescribed because they’re cheap and fast. Docs don’t care about delirium - they care about ticking the box and moving on. The FDA warning? Too little too late. I’ve seen 80-year-olds on 750mg of levo like it’s vitamin C. And now they’re in a nursing home. No one’s accountable. This isn’t medicine. It’s industrial negligence.
Oliver Calvert
February 18, 2026 AT 06:54Key point: stop the drug immediately. No waiting. No second opinions. If delirium pops up after starting a fluoroquinolone, pull it. Done. Beta-lactams are safer, cheaper, and just as effective for most infections. Why are we still using these neurotoxic options? I’ve seen it too many times - elderly patient, confused, no fever, no infection worsening - just started cipro 3 days ago. It’s obvious. But nobody connects the dots.
Haley DeWitt
February 18, 2026 AT 08:03OMG this is so important!! 😭 My grandma went through this and we had NO IDEA. She was screaming at the wall like there was a demon there. We thought it was dementia. Turns out it was levofloxacin. They didn’t even tell us it could do this. Please, please, please share this with everyone you know. I’m crying just thinking about it. 🥺
John Haberstroh
February 18, 2026 AT 11:41It’s funny how we treat antibiotics like candy. You got a cough? Here’s a big gun. You got a UTI? Take this nuclear option. Meanwhile, your brain’s getting hijacked. Fluoroquinolones are like a sledgehammer to a glass window - they work, but they shatter everything. And the worst part? The damage isn’t always visible on scans. It’s invisible until it’s too late. We need to stop being lazy with prescriptions.
Carrie Schluckbier
February 18, 2026 AT 21:28They’re doing this on purpose. The pharmaceutical industry knows these drugs cause brain damage. They’ve known for decades. The FDA update? A PR stunt. They don’t want you to know that your mom’s confusion was caused by a pill they made. They profit from nursing homes. They profit from long-term care. This isn’t negligence. It’s a calculated genocide of the elderly. Wake up.
Liam Earney
February 19, 2026 AT 16:08You know what breaks my heart? The silence. The way families just accept it - "Oh, grandpa’s just getting old." No. No, no, no. He was fine yesterday. Then came the antibiotic. Then came the terror. I’ve sat with people who stared at nothing, whispering to ghosts they didn’t know were real. And the doctors? They nod, write a note, and move on. I’ve cried so many times over this. Not because I’m weak - because this is cruelty disguised as care.
guy greenfeld
February 21, 2026 AT 01:37Think about it: we live in a world where a molecule - a single chemical structure - can unravel a human mind. Levofloxacin doesn’t care about your memories, your love, your laughter. It just slips into the brain like a thief in the night and flips the switch on GABA. And we call this medicine? No. This is alchemy gone wrong. We’re playing god with neurotransmitters and pretending we understand the soul. The real tragedy isn’t the delirium - it’s that we’re still surprised when the body rebels against our arrogance.